Articulations

Figure 9.1 Kayaking Without joints, body movements would be impossible. (credit: Graham Richardson/flickr.com)
Chapter Objectives
After this chapter, you will be able to:
- Discuss both functional and structural classifications for body joints
- Describe the characteristic features for fibrous, cartilaginous, and synovial joints and give examples of each
- Define and identify the different body movements
- Discuss the structure of specific body joints and the movements allowed by each
- Explain the development of body joints
Introduction
The adult human body has 206 bones, and with the exception of the hyoid bone in the neck, each bone is connected to at least one other bone. Joints or articulations are the location where bones come together. Many joints allow for movement between the bones. At these joints, the articulating surfaces of the adjacent bones can move smoothly against each other. However, the bones of other joints may be joined to each other by connective tissue or cartilage. These joints are designed for stability and provide for little or no movement. Importantly, joint stability and movement are related to each other. This means that stable joints allow for little or no mobility between the adjacent bones. Conversely, joints that provide the most movement between bones are the least stable. Understanding the relationship between joint structure and function will help to explain why particular types of joints are found in certain areas of the body.
The articulating surfaces of bones at stable types of joints, with little or no mobility, are strongly united to each other. For example, most of the joints of the skull are held together by fibrous connective tissue and do not allow for movement between the adjacent bones. This lack of mobility is important, because the skull bones serve to protect the brain. Similarly, other joints united by fibrous connective tissue allow for very little movement, which provides stability and weight-bearing support for the body. For example, the tibia and fibula of the leg are tightly united to give stability to the body when standing. At other joints, the bones are held together by cartilage, which permits limited movements between the bones. Thus, the joints of the vertebral column only allow for small movements between adjacent vertebrae, but when added together, these movements provide the flexibility that allows your body to twist, or bend to the front, back, or side. In contrast, at joints that allow for wide ranges of motion, the articulating surfaces of the bones are not directly united to each other. Instead, these surfaces are enclosed within a space filled with lubricating fluid, which allows the bones to move smoothly against each other. These joints provide greater mobility, but since the bones are free to move in relation to each other, the joint is less stable. Most of the joints between the bones of the appendicular skeleton are this freely moveable type of joint. These joints allow the muscles of the body to pull on a bone and thereby produce movement of that body region. Your ability to kick a soccer ball, pick up a fork, and dance the tango depend on mobility at these types of joints.
Classification of Joints
Learning Objectives
By the end of this section, you will be able to:
- Distinguish between the functional and structural classifications for joints
- Describe the three functional types of joints and give an example of each
- List the three types of diarthrodial joints
A joint, also called an articulation, is any place where adjacent bones or bone and cartilage come together (articulate with each other) to form a connection. Joints are classified both structurally and functionally. Structural classifications of joints take into account whether the adjacent bones are strongly anchored to each other by fibrous connective tissue or cartilage, or whether the adjacent bones articulate with each other within a fluid-filled space called a joint cavity. Functional classifications describe the degree of movement available between the bones, ranging from immobile, to slightly mobile, to freely moveable joints. The amount of movement available at a particular joint of the body is related to the functional requirements for that joint. Thus immobile or slightly moveable joints serve to protect internal organs, give stability to the body, and allow for limited body movement. In contrast, freely moveable joints allow for much more extensive movements of the body and limbs.
Structural Classification of Joints
The structural classification of joints is based on whether the articulating surfaces of the adjacent bones are directly connected by fibrous connective tissue or cartilage, or whether the articulating surfaces contact each other within a fluid-filled joint cavity. These differences serve to divide the joints of the body into three structural classifications. A fibrous joint is where the adjacent bones are united by fibrous connective tissue. At a cartilaginous joint, the bones are joined by hyaline cartilage or fibrocartilage. At a synovial joint, the articulating surfaces of the bones are not directly connected, but instead come into contact with each other within a joint cavity that is filled with a lubricating fluid. Synovial joints allow for free movement between the bones and are the most common joints of the body.
Functional Classification of Joints
The functional classification of joints is determined by the amount of mobility found between the adjacent bones. Joints are thus functionally classified as a synarthrosis or immobile joint, an amphiarthrosis or slightly moveable joint, or as a diarthrosis, which is a freely moveable joint (arthroun = “to fasten by a joint”). Depending on their location, fibrous joints may be functionally classified as a synarthrosis (immobile joint) or an amphiarthrosis (slightly mobile joint). Cartilaginous joints are also functionally classified as either a synarthrosis or an amphiarthrosis joint. All synovial joints are functionally classified as a diarthrosis joint.
Synarthrosis
An immobile or nearly immobile joint is called a synarthrosis. The immobile nature of these joints provide for a strong union between the articulating bones. This is important at locations where the bones provide protection for internal organs. Examples include sutures, the fibrous joints between the bones of the skull that surround and protect the brain (Figure 9.2), and the manubriosternal joint, the cartilaginous joint that unites the manubrium and body of the sternum for protection of the heart.
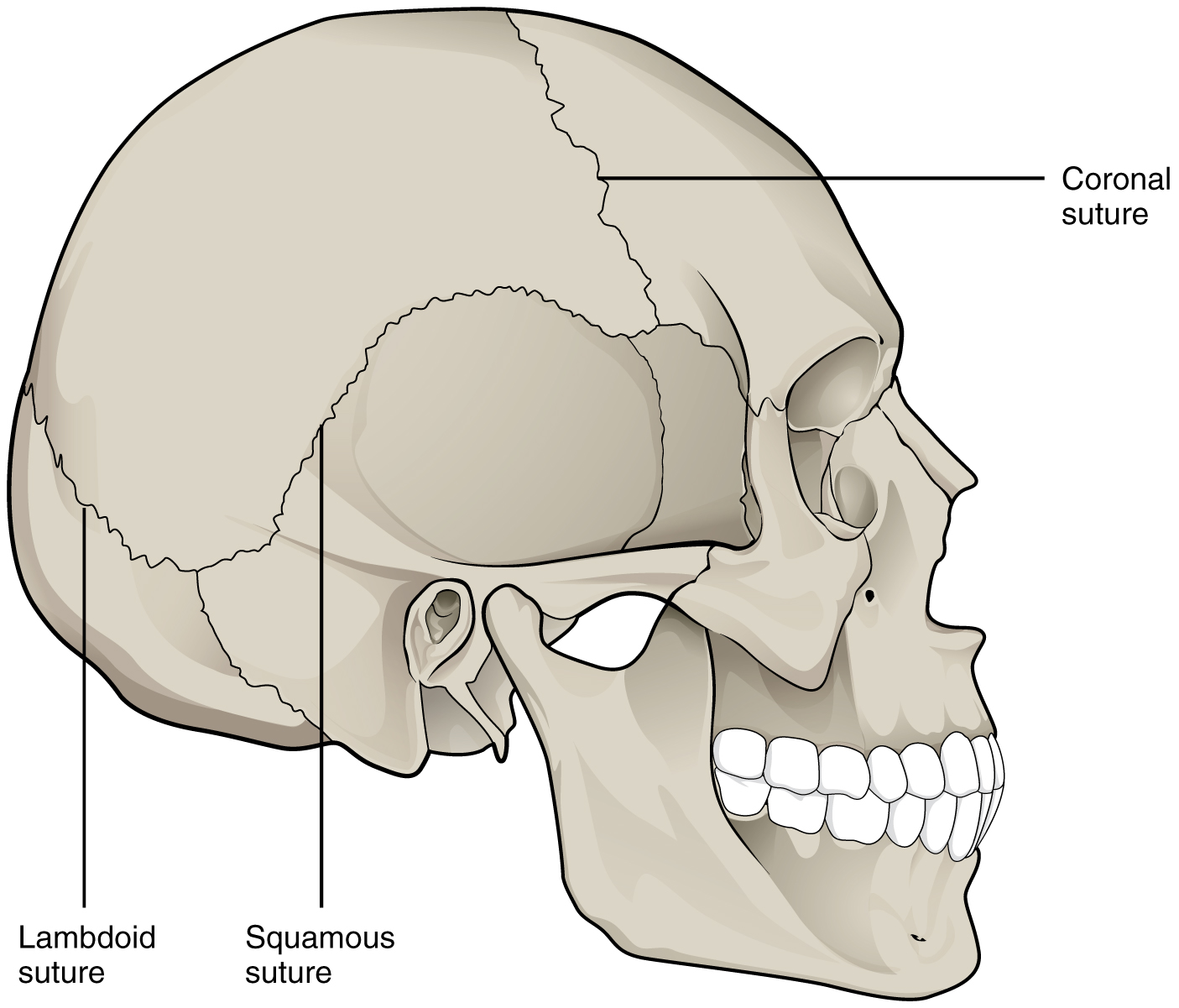
Figure 9.2 Suture Joints of Skull The suture joints of the skull are an example of a synarthrosis, an immobile or essentially immobile joint.
Amphiarthrosis
An amphiarthrosis is a joint that has limited mobility. An example of this type of joint is the cartilaginous joint that unites the bodies of adjacent vertebrae. Filling the gap between the vertebrae is a thick pad of fibrocartilage called an intervertebral disc (Figure 9.3). Each intervertebral disc strongly unites the vertebrae but still allows for a limited amount of movement between them. However, the small movements available between adjacent vertebrae can sum together along the length of the vertebral column to provide for large ranges of body movements.
Another example of an amphiarthrosis is the pubic symphysis of the pelvis. This is a cartilaginous joint in which the pubic regions of the right and left hip bones are strongly anchored to each other by fibrocartilage. This joint normally has very little mobility. The strength of the pubic symphysis is important in conferring weight-bearing stability to the pelvis.
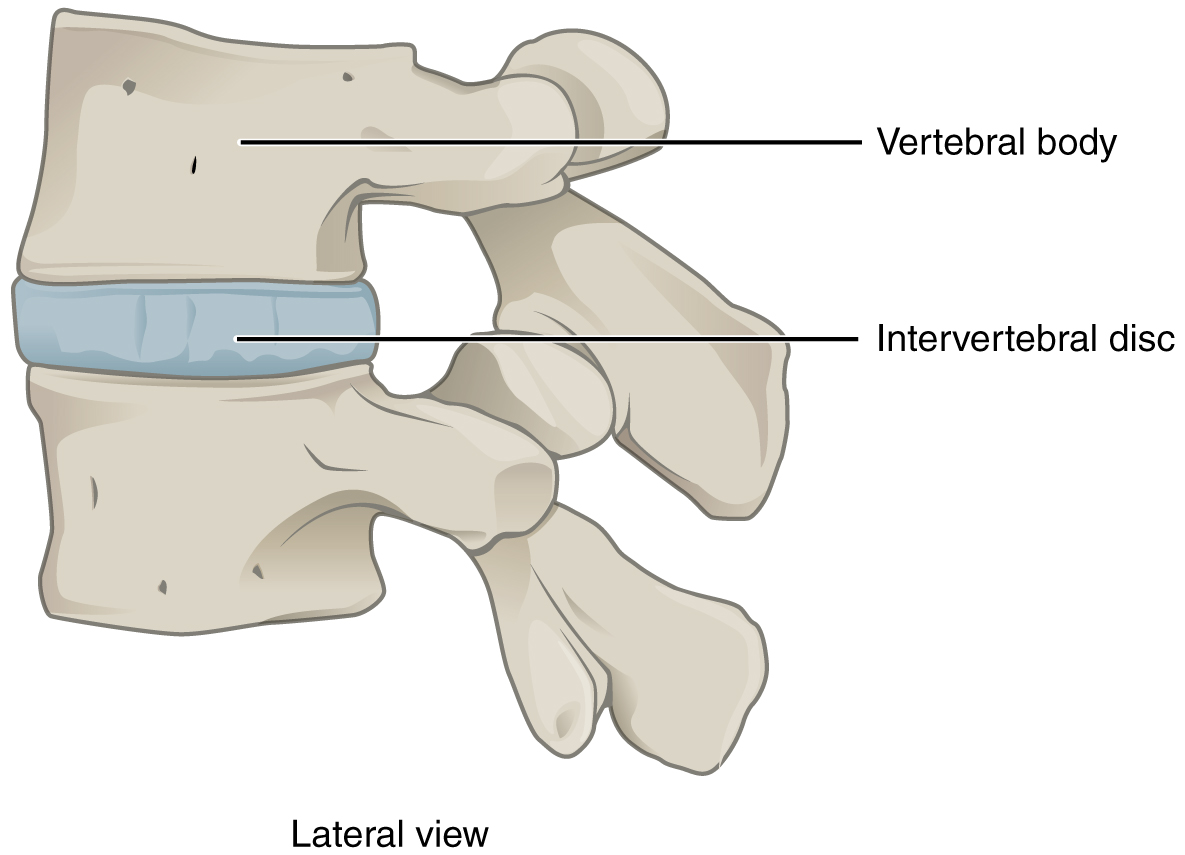
Figure 9.3 Intervertebral Disc An intervertebral disc unites the bodies of adjacent vertebrae within the vertebral column. Each disc allows for limited movement between the vertebrae and thus functionally forms an amphiarthrosis type of joint. Intervertebral discs are made of fibrocartilage and thereby structurally form a symphysis type of cartilaginous joint.
Diarthrosis
A freely mobile joint is classified as a diarthrosis. These types of joints include all synovial joints of the body, which provide the majority of body movements. Most diarthrotic joints are found in the appendicular skeleton and thus give the limbs a wide range of motion. These joints are divided into three categories, based on the number of axes of motion provided by each. An axis in anatomy is described as the movements in reference to the three anatomical planes: transverse, frontal, and sagittal. Thus, diarthroses are classified as uniaxial (for movement in one plane), biaxial (for movement in two planes), or multiaxial joints (for movement in all three anatomical planes).
A uniaxial joint only allows for a motion in a single plane (around a single axis). The elbow joint, which only allows for bending or straightening, is an example of a uniaxial joint. A biaxial joint allows for motions within two planes. An example of a biaxial joint is a metacarpophalangeal joint (knuckle joint) of the hand. The joint allows for movement along one axis to produce bending or straightening of the finger, and movement along a second axis, which allows for spreading of the fingers away from each other and bringing them together. A joint that allows for the several directions of movement is called a multiaxial joint (polyaxial or triaxial joint). This type of diarthrotic joint allows for movement along three axes (Figure 9.4). The shoulder and hip joints are multiaxial joints. They allow the upper or lower limb to move in an anterior-posterior direction and a medial-lateral direction. In addition, the limb can also be rotated around its long axis. This third movement results in rotation of the limb so that its anterior surface is moved either toward or away from the midline of the body.
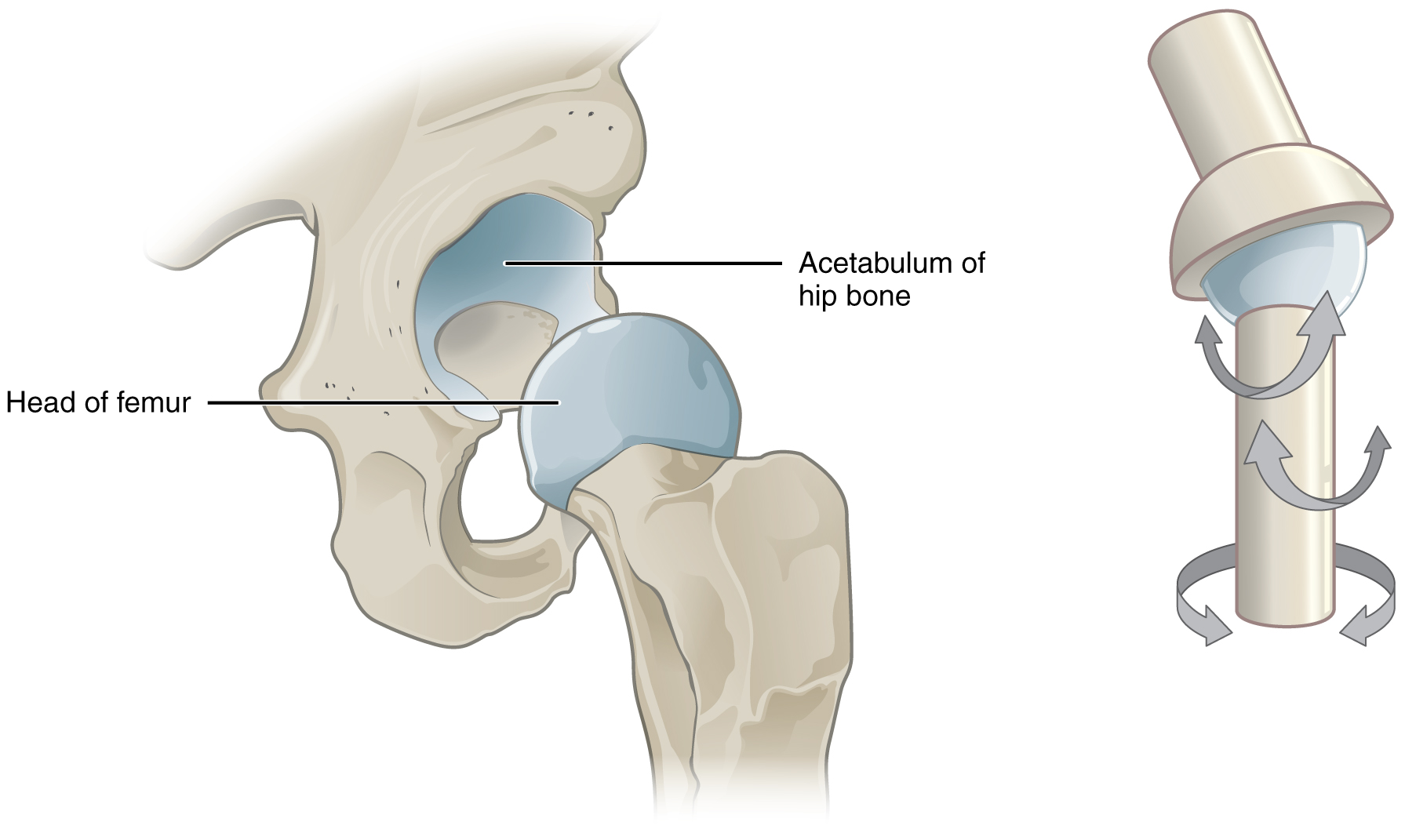
Figure 9.4 Multiaxial Joint A multiaxial joint, such as the hip joint, allows for three types of movement: anterior-posterior, medial-lateral, and rotational.
Fibrous Joints
Learning Objectives
By the end of this section, you will be able to:
- Describe the structural features of fibrous joints
- Distinguish between a suture, syndesmosis, and gomphosis
- Give an example of each type of fibrous joint
At a fibrous joint, the adjacent bones are directly connected to each other by fibrous connective tissue, and thus the bones do not have a joint cavity between them (Figure 9.5). The gap between the bones may be narrow or wide. There are three types of fibrous joints. A suture is the narrow fibrous joint found between most bones of the skull. At a syndesmosis joint, the bones are more widely separated but are held together by a narrow band of fibrous connective tissue called a ligament or a wide sheet of connective tissue called an interosseous membrane. This type of fibrous joint is found between the shaft regions of the long bones in the forearm and in the leg. Lastly, a gomphosis is the narrow fibrous joint between the roots of a tooth and the bony socket in the jaw into which the tooth fits.
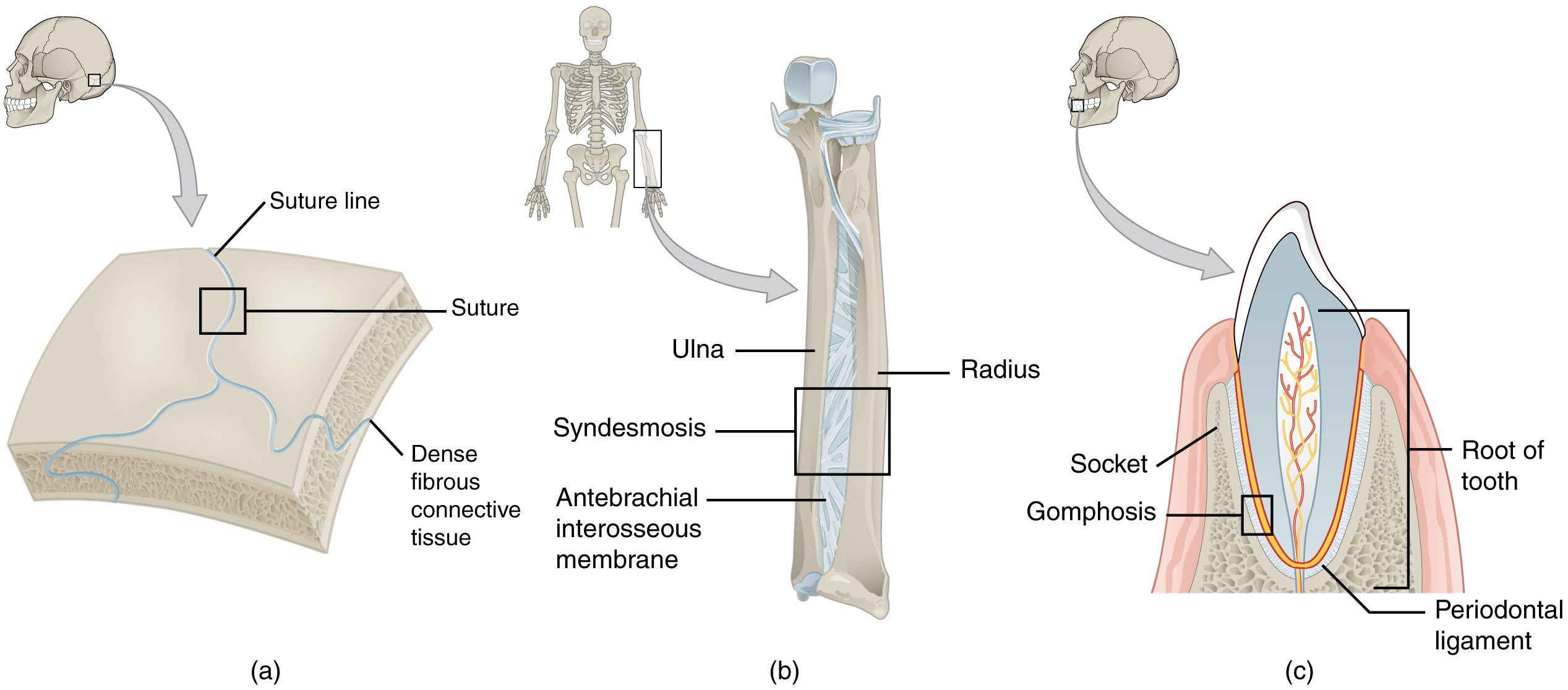
Figure 9.5 Fibrous Joints Fibrous joints form strong connections between bones. (a) Sutures join most bones of the skull. (b) An interosseous membrane forms a syndesmosis between the radius and ulna bones of the forearm. (c) A gomphosis is a specialized fibrous joint that anchors a tooth to its socket in the jaw.
Suture
All the bones of the skull, except for the mandible, are joined to each other by a fibrous joint called a suture. The fibrous connective tissue found at a suture (“to bind or sew”) strongly unites the adjacent skull bones and thus helps to protect the brain and form the face. In adults, the skull bones are closely opposed and fibrous connective tissue fills the narrow gap between the bones. The suture is frequently convoluted, forming a tight union that prevents most movement between the bones. (See Figure 9.5a.) Thus, skull sutures are functionally classified as a synarthrosis, although some sutures may allow for slight movements between the cranial bones.
In newborns and infants, the areas of connective tissue between the bones are much wider, especially in those areas on the top and sides of the skull that will become the sagittal, coronal, squamous, and lambdoid sutures. These broad areas of connective tissue are called fontanelles (Figure 9.6). During birth, the fontanelles provide flexibility to the skull, allowing the bones to push closer together or to overlap slightly, thus aiding movement of the infant’s head through the birth canal. After birth, these expanded regions of connective tissue allow for rapid growth of the skull and enlargement of the brain. The fontanelles greatly decrease in width during the first year after birth as the skull bones enlarge. When the connective tissue between the adjacent bones is reduced to a narrow layer, these fibrous joints are now called sutures. At some sutures, the connective tissue will ossify and be converted into bone, causing the adjacent bones to fuse to each other. This fusion between bones is called a synostosis (“joined by bone”). Examples of synostosis fusions between cranial bones are found both early and late in life. At the time of birth, the frontal and maxillary bones consist of right and left halves joined together by sutures, which disappear by the eighth year as the halves fuse together to form a single bone. Late in life, the sagittal, coronal, and lambdoid sutures of the skull will begin to ossify and fuse, causing the suture line to gradually disappear.
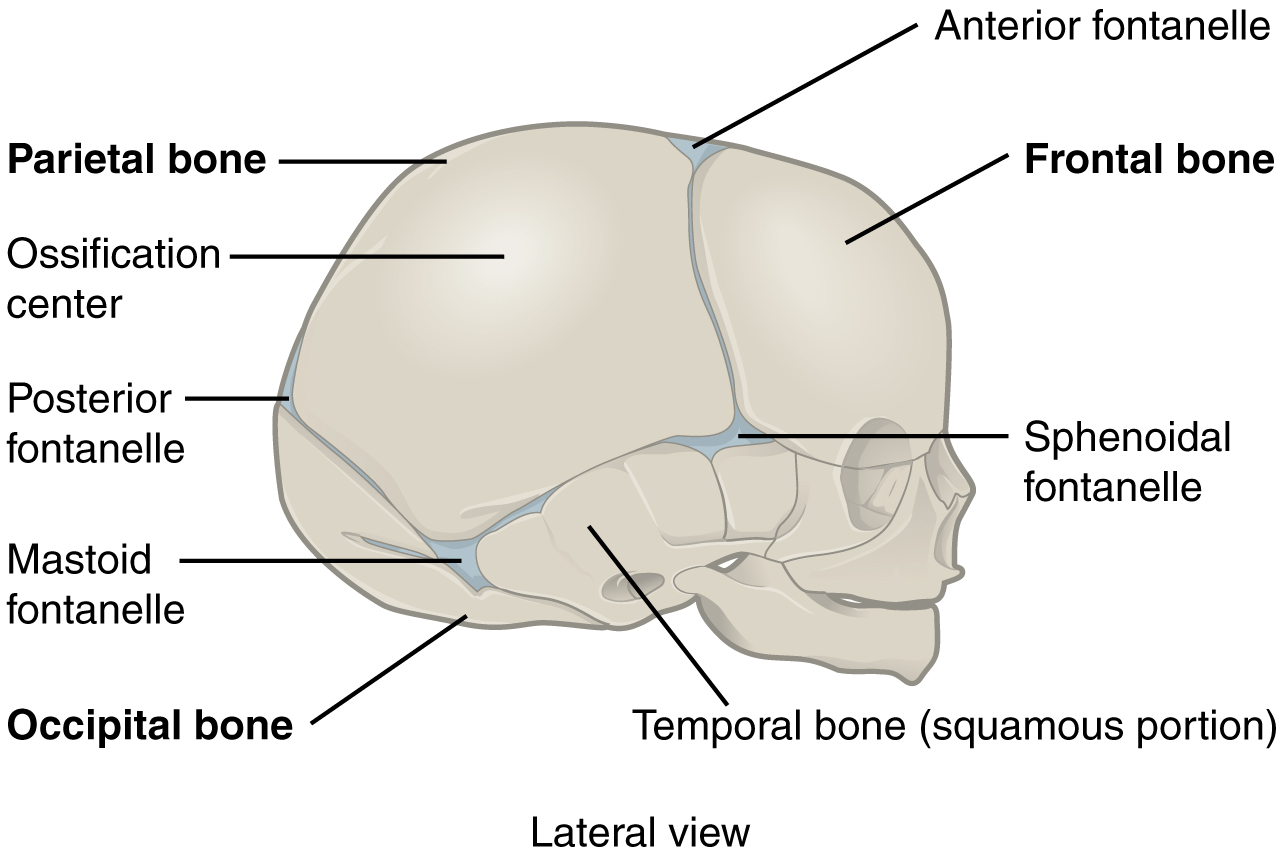
Figure 9.6 The Newborn Skull The fontanelles of a newborn’s skull are broad areas of fibrous connective tissue that form fibrous joints between the bones of the skull.
Cartilaginous Joints
Learning Objectives
By the end of this section, you will be able to:
- Describe the structural features of cartilaginous joints
- Give an example of each type of cartilaginous joint
As the name indicates, at a cartilaginous joint, the adjacent bones are united by cartilage, a tough but flexible type of connective tissue. These types of joints lack a joint cavity and involve bones that are joined together by either hyaline cartilage or fibrocartilage (Figure 9.7). There are two types of cartilaginous joints. A synchondrosis is a cartilaginous joint where the bones are joined by hyaline cartilage. Also classified as a synchondrosis are places where bone is united to a cartilage structure, such as between the anterior end of a rib and the costal cartilage of the thoracic cage. The second type of cartilaginous joint is a symphysis, where the bones are joined by fibrocartilage.
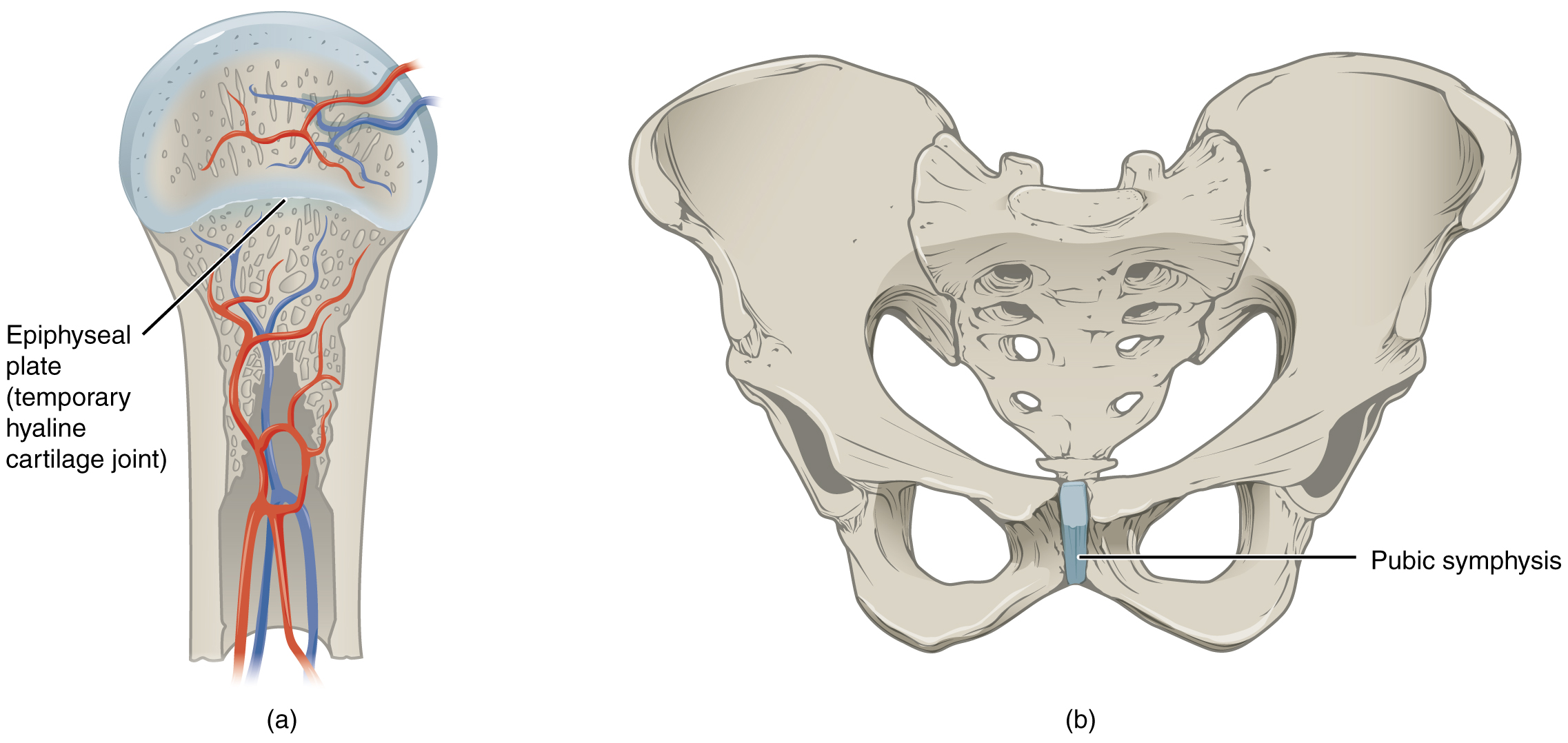
Figure 9.7 Cartilaginous Joints At cartilaginous joints, bones are united by hyaline cartilage to form a synchondrosis or by fibrocartilage to form a symphysis. (a) The hyaline cartilage of the epiphyseal plate (growth plate) forms a synchondrosis that unites the shaft (diaphysis) and end (epiphysis) of a long bone and allows the bone to grow in length. (b) The pubic portions of the right and left hip bones of the pelvis are joined together by fibrocartilage, forming the pubic symphysis.
Epiphyseal Plate (Synchondrosis)
A synchondrosis (“joined by cartilage”) is a cartilaginous joint where bones are joined together by hyaline cartilage, or where bone is united to hyaline cartilage. A synchondrosis may be temporary or permanent. A temporary synchondrosis is the epiphyseal plate (growth plate) of a growing long bone. The epiphyseal plate is the region of growing hyaline cartilage that unites the diaphysis (shaft) of the bone to the epiphysis (end of the bone). Bone lengthening involves growth of the epiphyseal plate cartilage and its replacement by bone, which adds to the diaphysis. For many years during childhood growth, the rates of cartilage growth and bone formation are equal and thus the epiphyseal plate does not change in overall thickness as the bone lengthens. During the late teens and early 20s, growth of the cartilage slows and eventually stops. The epiphyseal plate is then completely replaced by bone, and the diaphysis and epiphysis portions of the bone fuse together to form a single adult bone. This fusion of the diaphysis and epiphysis is a synostosis. Once this occurs, bone lengthening ceases. For this reason, the epiphyseal plate is considered to be a temporary synchondrosis. Because cartilage is softer than bone tissue, injury to a growing long bone can damage the epiphyseal plate cartilage, thus stopping bone growth and preventing additional bone lengthening.
Growing layers of cartilage also form synchondroses that join together the ilium, ischium, and pubic portions of the hip bone during childhood and adolescence. When body growth stops, the cartilage disappears and is replaced by bone, forming synostoses and fusing the bony components together into the single hip bone of the adult. Similarly, synostoses unite the sacral vertebrae that fuse together to form the adult sacrum.
Interactive Link
Visit this website to view a radiograph (X-ray image) of a child’s hand and wrist. The growing bones of child have an epiphyseal plate that forms a synchondrosis between the shaft and end of a long bone. Being less dense than bone, the area of epiphyseal cartilage is seen on this radiograph as the dark epiphyseal gaps located near the ends of the long bones, including the radius, ulna, metacarpal, and phalanx bones. Which of the bones in this image do not show an epiphyseal plate (epiphyseal gap)?
Symphysis and Intervertebral Discs
A cartilaginous joint where the bones are joined by fibrocartilage is called a symphysis (“growing together”). Fibrocartilage is very strong because it contains numerous bundles of thick collagen fibers, thus giving it a much greater ability to resist pulling and bending forces when compared with hyaline cartilage. This gives symphyses the ability to strongly unite the adjacent bones, but can still allow for limited movement to occur. Thus, a symphysis is functionally classified as an amphiarthrosis.
The gap separating the bones at a symphysis may be narrow or wide. Examples in which the gap between the bones is narrow include the pubic symphysis and the manubriosternal joint. At the pubic symphysis, the pubic portions of the right and left hip bones of the pelvis are joined together by fibrocartilage across a narrow gap.
The intervertebral symphysis is a wide symphysis located between the bodies of adjacent vertebrae of the vertebral column. Here a thick pad of fibrocartilage called an intervertebral disc strongly unites the adjacent vertebrae by filling the gap between them. The width of the intervertebral symphysis is important because it allows for small movements between the adjacent vertebrae. In addition, the thick intervertebral disc provides cushioning between the vertebrae, which is important when carrying heavy objects or during high-impact activities such as running or jumping.
Synovial Joints
Learning Objectives
By the end of this section, you will be able to:
- Describe the structural features of a synovial joint
- Discuss the function of additional structures associated with synovial joints
Synovial joints are the most common type of joint in the body (Figure 9.8). A key structural characteristic for a synovial joint that is not seen at fibrous or cartilaginous joints is the presence of a joint cavity. This fluid-filled space is the site at which the articulating surfaces of the bones contact each other. Also unlike fibrous or cartilaginous joints, the articulating bone surfaces at a synovial joint are not directly connected to each other with fibrous connective tissue or cartilage. This gives the bones of a synovial joint the ability to move smoothly against each other, allowing for increased joint mobility.
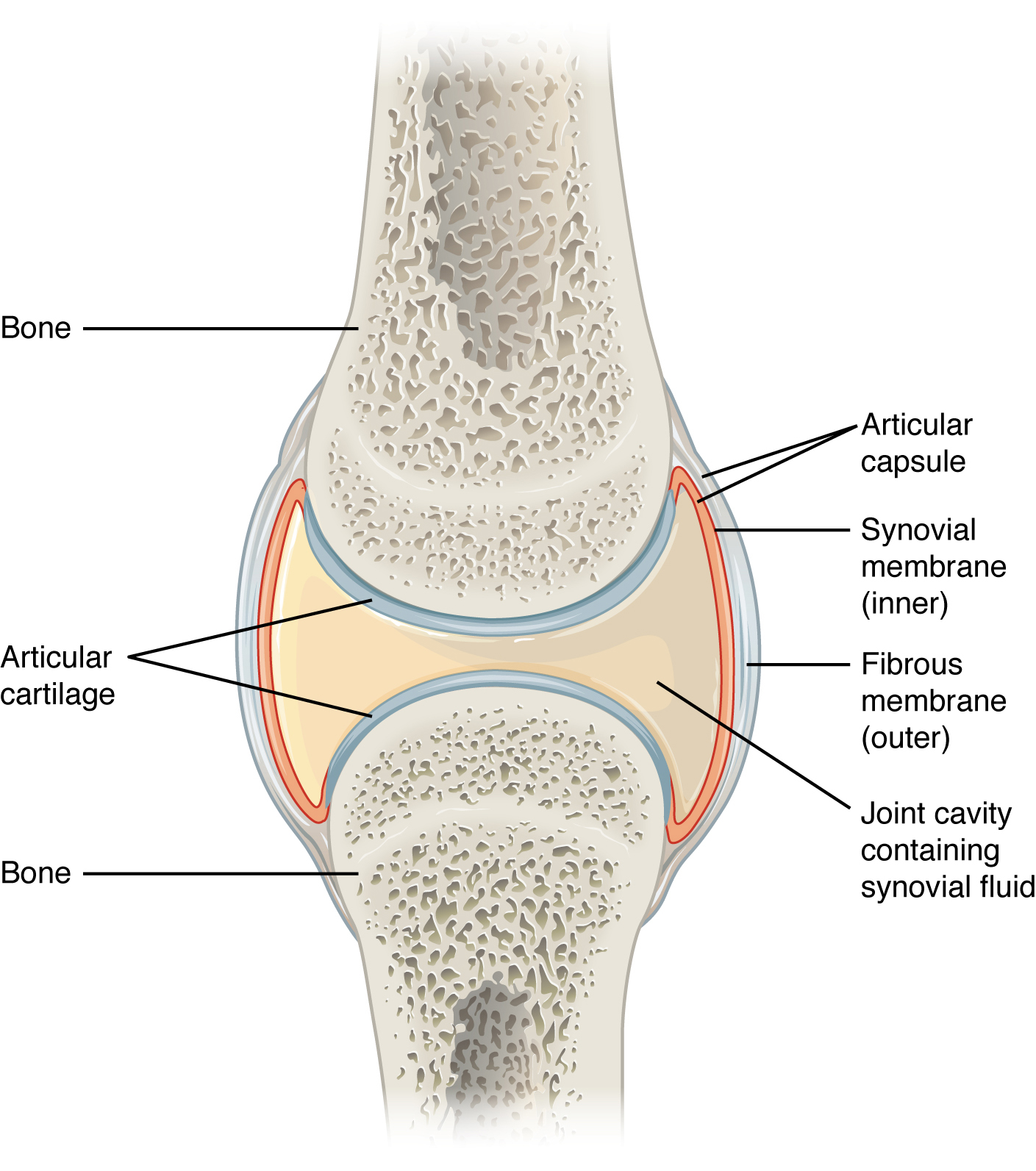
Figure 9.8 Synovial Joints Synovial joints allow for smooth movements between the adjacent bones. The joint is surrounded by an articular capsule that defines a joint cavity filled with synovial fluid. The articulating surfaces of the bones are covered by a thin layer of articular cartilage. Ligaments support the joint by holding the bones together and resisting excess or abnormal joint motions.
Structural Features of Synovial Joints
Synovial joints are characterized by the presence of a joint cavity. The walls of this space are formed by the articular capsule, a fibrous connective tissue structure that is attached to each bone just outside the area of the bone’s articulating surface. The bones of the joint articulate with each other within the joint cavity.
Friction between the bones at a synovial joint is prevented by the presence of the articular cartilage, a thin layer of hyaline cartilage that covers the entire articulating surface of each bone. However, unlike at a cartilaginous joint, the articular cartilages of each bone are not continuous with each other. Instead, the articular cartilage acts like a Teflon® coating over the bone surface, allowing the articulating bones to move smoothly against each other without damaging the underlying bone tissue. Lining the inner surface of the articular capsule is a thin synovial membrane. The cells of this membrane secrete synovial fluid (synovia = “a thick fluid”), a thick, slimy fluid that provides lubrication to further reduce friction between the bones of the joint. This fluid also provides nourishment to the articular cartilage, which does not contain blood vessels. The ability of the bones to move smoothly against each other within the joint cavity, and the freedom of joint movement this provides, means that each synovial joint is functionally classified as a diarthrosis.
Outside of their articulating surfaces, the bones are connected together by ligaments, which are strong bands of fibrous connective tissue. These strengthen and support the joint by anchoring the bones together and preventing their separation. Ligaments allow for normal movements at a joint, but limit the range of these motions, thus preventing excessive or abnormal joint movements. Ligaments are classified based on their relationship to the fibrous articular capsule. An extrinsic ligament is located outside of the articular capsule, an intrinsic ligament is fused to or incorporated into the wall of the articular capsule, and an intracapsular ligament is located inside of the articular capsule.
At many synovial joints, additional support is provided by the muscles and their tendons that act across the joint. A tendon is the dense connective tissue structure that attaches a muscle to bone. As forces acting on a joint increase, the body will automatically increase the overall strength of contraction of the muscles crossing that joint, thus allowing the muscle and its tendon to serve as a “dynamic ligament” to resist forces and support the joint. This type of indirect support by muscles is very important at the shoulder joint, for example, where the ligaments are relatively weak.
Additional Structures Associated with Synovial Joints
A few synovial joints of the body have a fibrocartilage structure located between the articulating bones. This is called an articular disc, which is generally small and oval-shaped, or a meniscus, which is larger and C-shaped. These structures can serve several functions, depending on the specific joint. In some places, an articular disc may act to strongly unite the bones of the joint to each other. Examples of this include the articular discs found at the sternoclavicular joint or between the distal ends of the radius and ulna bones. At other synovial joints, the disc can provide shock absorption and cushioning between the bones, which is the function of each meniscus within the knee joint. Finally, an articular disc can serve to smooth the movements between the articulating bones, as seen at the temporomandibular joint. Some synovial joints also have a fat pad, which can serve as a cushion between the bones.
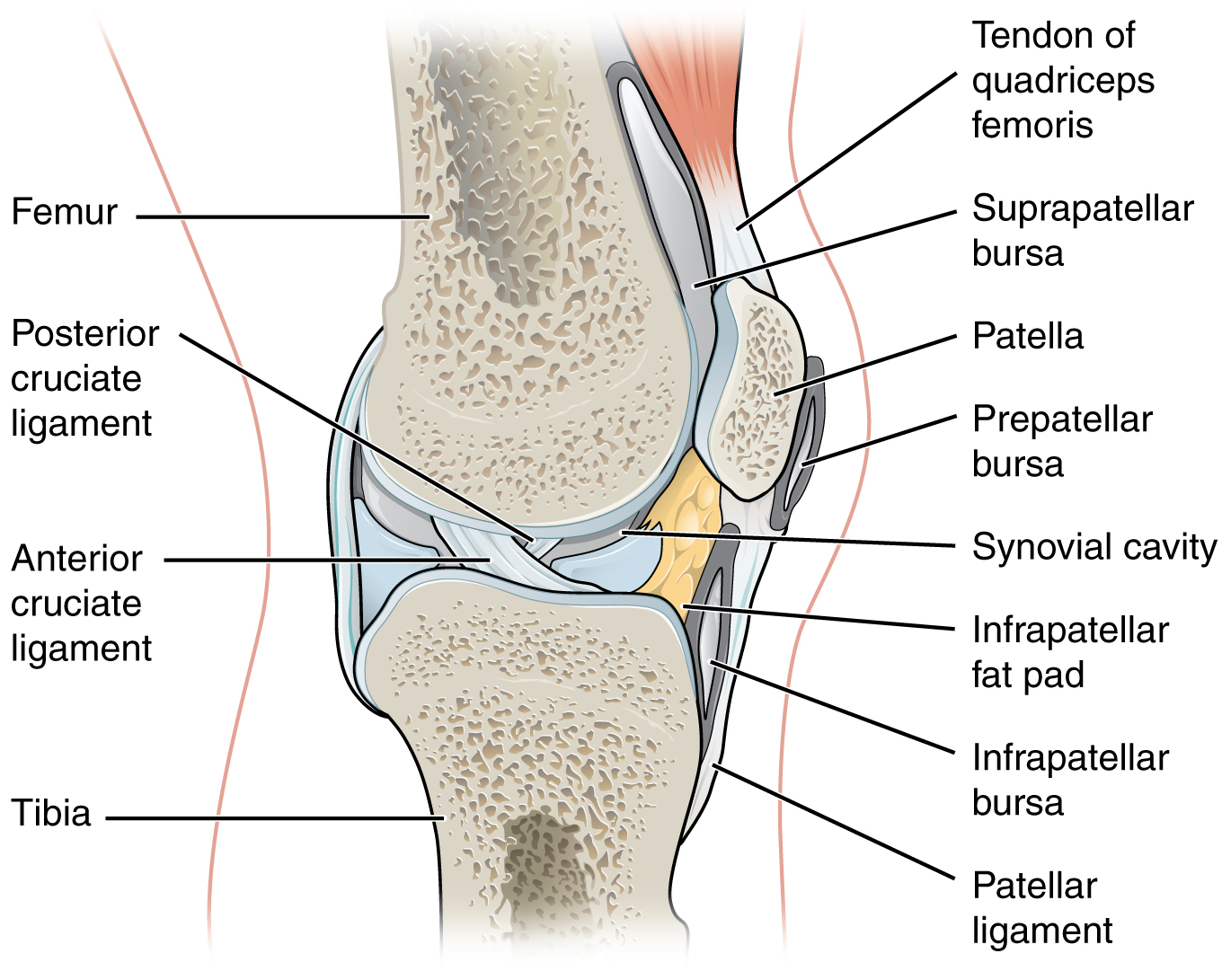
Figure 9.9 Bursae Bursae are fluid-filled sacs that serve to prevent friction between skin, muscle, or tendon and an underlying bone. Three major bur
Types of Synovial Joints
Synovial joints are subdivided based on the shapes of the articulating surfaces of the bones that form each joint. The six types of synovial joints are pivot, hinge, condyloid, saddle, plane, and ball-and socket-joints (Figure 9.10).
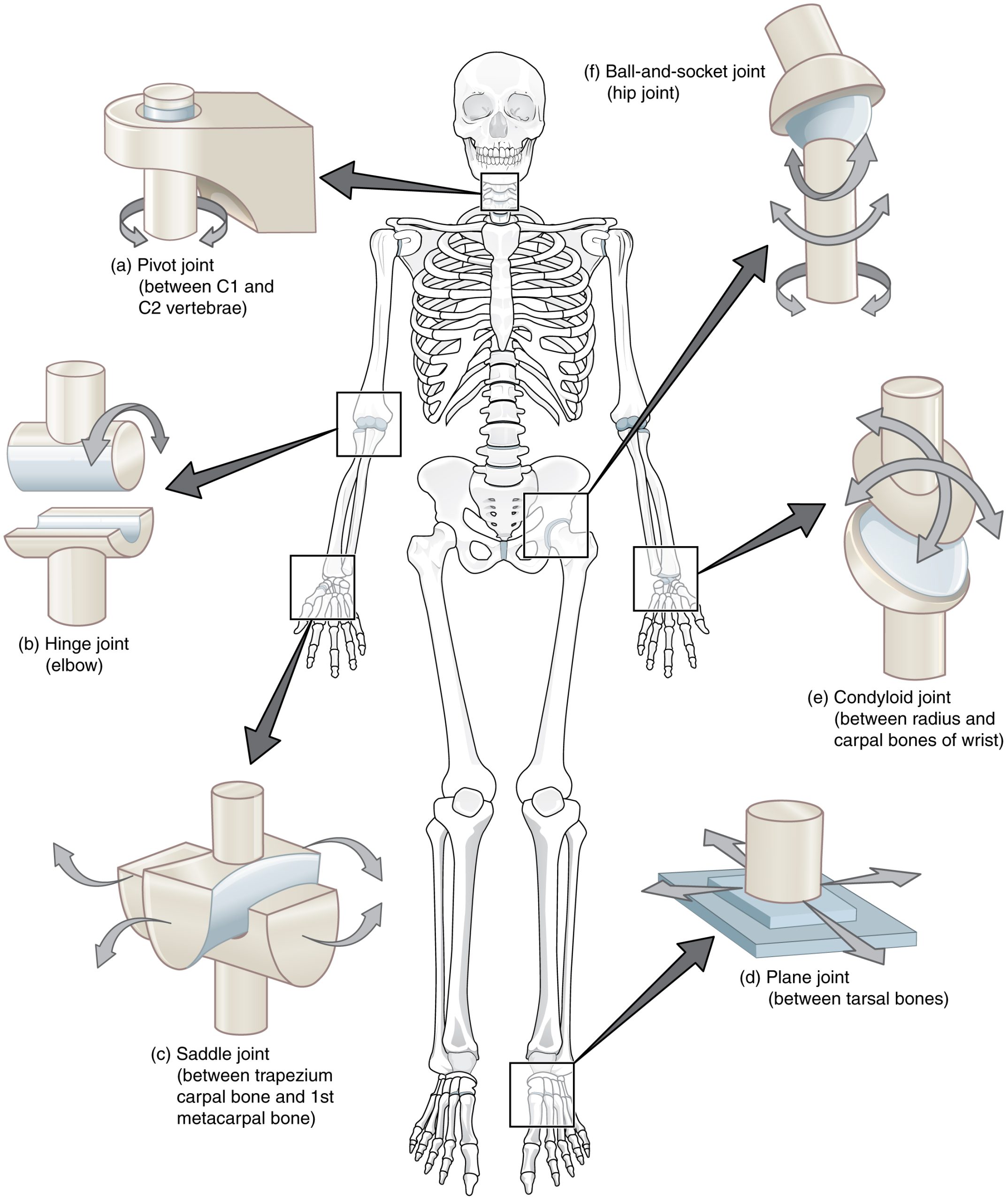
Figure 9.10 Types of Synovial Joints The six types of synovial joints allow the body to move in a variety of ways. (a) Pivot joints allow for rotation around an axis, such as between the first and second cervical vertebrae, which allows for side-to-side rotation of the head. (b) The hinge joint of the elbow works like a door hinge. (c) The articulation between the trapezium carpal bone and the first metacarpal bone at the base of the thumb is a saddle joint. (d) Plane joints, such as those between the tarsal bones of the foot, allow for limited gliding movements between bones. (e) The radiocarpal joint of the wrist is a condyloid joint. (f) The hip and shoulder joints are the only ball-and-socket joints of the body.
Pivot Joint
At a pivot joint, a rounded portion of a bone is enclosed within a ring formed partially by the articulation with another bone and partially by a ligament (see Figure 9.10a). The bone rotates within this ring. Since the rotation is around a single axis, pivot joints are functionally classified as a uniaxial diarthrosis type of joint. An example of a pivot joint is the atlantoaxial joint, found between the C1 (atlas) and C2 (axis) vertebrae. Here, the upward projecting dens of the axis articulates with the inner aspect of the atlas, where it is held in place by a ligament. Rotation at this joint allows you to turn your head from side to side. A second pivot joint is found at the proximal radioulnar joint. Here, the head of the radius is largely encircled by a ligament that holds it in place as it articulates with the radial notch of the ulna. Rotation of the radius allows for forearm movements.
Hinge Joint
In a hinge joint, the convex end of one bone articulates with the concave end of the adjoining bone (see Figure 9.10b). This type of joint allows only for bending and straightening motions along a single axis, and thus hinge joints are functionally classified as uniaxial joints. A good example is the elbow joint, with the articulation between the trochlea of the humerus and the trochlear notch of the ulna. Other hinge joints of the body include the knee, ankle, and interphalangeal joints between the phalanx bones of the fingers and toes.
Condyloid Joint
At a condyloid joint (ellipsoid joint), the shallow depression at the end of one bone articulates with a rounded structure from an adjacent bone or bones (see Figure 9.10e). The knuckle (metacarpophalangeal) joints of the hand between the distal end of a metacarpal bone and the proximal phalanx bone are condyloid joints. Another example is the radiocarpal joint of the wrist, between the shallow depression at the distal end of the radius bone and the rounded scaphoid, lunate, and triquetrum carpal bones. In this case, the articulation area has a more oval (elliptical) shape. Functionally, condyloid joints are biaxial joints that allow for two planes of movement. One movement involves the bending and straightening of the fingers or the anterior-posterior movements of the hand. The second movement is a side-to-side movement, which allows you to spread your fingers apart and bring them together, or to move your hand in a medial-going or lateral-going direction.
Saddle Joint
At a saddle joint, both of the articulating surfaces for the bones have a saddle shape, which is concave in one direction and convex in the other (see Figure 9.10c). This allows the two bones to fit together like a rider sitting on a saddle. Saddle joints are functionally classified as biaxial joints. The primary example is the first carpometacarpal joint, between the trapezium (a carpal bone) and the first metacarpal bone at the base of the thumb. This joint provides the thumb the ability to move away from the palm of the hand along two planes. Thus, the thumb can move within the same plane as the palm of the hand, or it can jut out anteriorly, perpendicular to the palm. This movement of the first carpometacarpal joint is what gives humans their distinctive “opposable” thumbs. The sternoclavicular joint is also classified as a saddle joint.
Plane Joint
At a plane joint (gliding joint), the articulating surfaces of the bones are flat or slightly curved and of approximately the same size, which allows the bones to slide against each other (see Figure 9.10d). The motion at this type of joint is usually small and tightly constrained by surrounding ligaments. Based only on their shape, plane joints can allow multiple movements, including rotation. Thus plane joints can be functionally classified as a multiaxial joint. However, not all of these movements are available to every plane joint due to limitations placed on it by ligaments or neighboring bones. Thus, depending upon the specific joint of the body, a plane joint may exhibit only a single type of movement or several movements. Plane joints are found between the carpal bones (intercarpal joints) of the wrist or tarsal bones (intertarsal joints) of the foot, between the clavicle and acromion of the scapula (acromioclavicular joint), and between the superior and inferior articular processes of adjacent vertebrae (zygapophysial joints).
Ball-and-Socket Joint
The joint with the greatest range of motion is the ball-and-socket joint. At these joints, the rounded head of one bone (the ball) fits into the concave articulation (the socket) of the adjacent bone (see Figure 9.10f). The hip joint and the glenohumeral (shoulder) joint are the only ball-and-socket joints of the body. At the hip joint, the head of the femur articulates with the acetabulum of the hip bone, and at the shoulder joint, the head of the humerus articulates with the glenoid cavity of the scapula.
Ball-and-socket joints are classified functionally as multiaxial joints. The femur and the humerus are able to move in both anterior-posterior and medial-lateral directions and they can also rotate around their long axis. The shallow socket formed by the glenoid cavity allows the shoulder joint an extensive range of motion. In contrast, the deep socket of the acetabulum and the strong supporting ligaments of the hip joint serve to constrain movements of the femur, reflecting the need for stability and weight-bearing ability at the hip.
Interactive Link
Watch this video to see an animation of synovial joints in action. Synovial joints are places where bones articulate with each other inside of a joint cavity. The different types of synovial joints are the ball-and-socket joint (shoulder joint), hinge joint (knee), pivot joint (atlantoaxial joint, between C1 and C2 vertebrae of the neck), condyloid joint (radiocarpal joint of the wrist), saddle joint (first carpometacarpal joint, between the trapezium carpal bone and the first metacarpal bone, at the base of the thumb), and plane joint (facet joints of vertebral column, between superior and inferior articular processes). Which type of synovial joint allows for the widest range of motion?
Aging and the…Joints
Arthritis is a common disorder of synovial joints that involves inflammation of the joint. This often results in significant joint pain, along with swelling, stiffness, and reduced joint mobility. There are more than 100 different forms of arthritis. Arthritis may arise from aging, damage to the articular cartilage, autoimmune diseases, bacterial or viral infections, or unknown (probably genetic) causes.
The most common type of arthritis is osteoarthritis, which is associated with aging and “wear and tear” of the articular cartilage (Figure 9.11). Risk factors that may lead to osteoarthritis later in life include injury to a joint; jobs that involve physical labor; sports with running, twisting, or throwing actions; and being overweight. These factors put stress on the articular cartilage that covers the surfaces of bones at synovial joints, causing the cartilage to gradually become thinner. As the articular cartilage layer wears down, more pressure is placed on the bones. The joint responds by increasing production of the lubricating synovial fluid, but this can lead to swelling of the joint cavity, causing pain and joint stiffness as the articular capsule is stretched. The bone tissue underlying the damaged articular cartilage also responds by thickening, producing irregularities and causing the articulating surface of the bone to become rough or bumpy. Joint movement then results in pain and inflammation. In its early stages, symptoms of osteoarthritis may be reduced by mild activity that “warms up” the joint, but the symptoms may worsen following exercise. In individuals with more advanced osteoarthritis, the affected joints can become more painful and therefore are difficult to use effectively, resulting in increased immobility. There is no cure for osteoarthritis, but several treatments can help alleviate the pain. Treatments may include lifestyle changes, such as weight loss and low-impact exercise, and over-the-counter or prescription medications that help to alleviate the pain and inflammation. For severe cases, joint replacement surgery (arthroplasty) may be required.
Joint replacement is a very invasive procedure, so other treatments are always tried before surgery. However arthroplasty can provide relief from chronic pain and can enhance mobility within a few months following the surgery. This type of surgery involves replacing the articular surfaces of the bones with prosthesis (artificial components). For example, in hip arthroplasty, the worn or damaged parts of the hip joint, including the head and neck of the femur and the acetabulum of the pelvis, are removed and replaced with artificial joint components. The replacement head for the femur consists of a rounded ball attached to the end of a shaft that is inserted inside the diaphysis of the femur. The acetabulum of the pelvis is reshaped and a replacement socket is fitted into its place. The parts, which are always built in advance of the surgery, are sometimes custom made to produce the best possible fit for a patient.
Gout is a form of arthritis that results from the deposition of uric acid crystals within a body joint. Usually only one or a few joints are affected, such as the big toe, knee, or ankle. The attack may only last a few days, but may return to the same or another joint. Gout occurs when the body makes too much uric acid or the kidneys do not properly excrete it. A diet with excessive fructose has been implicated in raising the chances of a susceptible individual developing gout.
Other forms of arthritis are associated with various autoimmune diseases, bacterial infections of the joint, or unknown genetic causes. Autoimmune diseases, including rheumatoid arthritis, scleroderma, or systemic lupus erythematosus, produce arthritis because the immune system of the body attacks the body joints. In rheumatoid arthritis, the joint capsule and synovial membrane become inflamed. As the disease progresses, the articular cartilage is severely damaged or destroyed, resulting in joint deformation, loss of movement, and severe disability. The most commonly involved joints are the hands, feet, and cervical spine, with corresponding joints on both sides of the body usually affected, though not always to the same extent. Rheumatoid arthritis is also associated with lung fibrosis, vasculitis (inflammation of blood vessels), coronary heart disease, and premature mortality. With no known cure, treatments are aimed at alleviating symptoms. Exercise, anti-inflammatory and pain medications, various specific disease-modifying anti-rheumatic drugs, or surgery are used to treat rheumatoid arthritis.
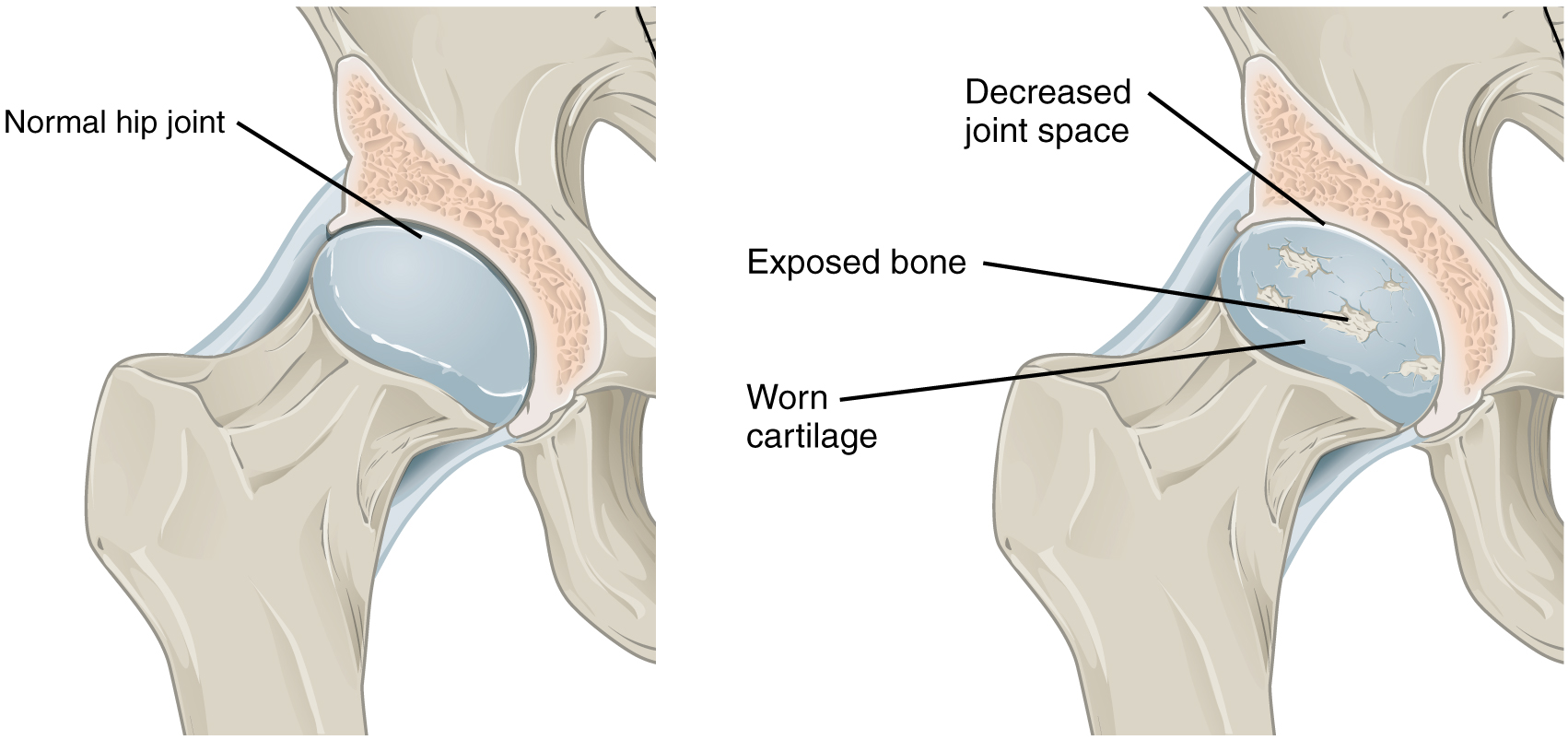
Figure 9.11 Osteoarthritis Osteoarthritis of a synovial joint results from aging or prolonged joint wear and tear. These cause erosion and loss of the articular cartilage covering the surfaces of the bones, resulting in inflammation that causes joint stiffness and pain.
Interactive Link
Visit this website to learn about a patient who arrives at the hospital with joint pain and weakness in his legs. What caused this patient’s weakness?
Interactive Link
Watch this animation to observe hip replacement surgery (total hip arthroplasty), which can be used to alleviate the pain and loss of joint mobility associated with osteoarthritis of the hip joint. What is the most common cause of hip disability?
Interactive Link
Watch this video to learn about the symptoms and treatments for rheumatoid arthritis. Which system of the body malfunctions in rheumatoid arthritis and what does this cause?
Anatomy of the Knee Joint
Learning Objectives
By the end of this section, you will be able to:
- Describe the bones that articulate together to form the knee joint
- Discuss the movements available at each joint
- Describe the structures that support and prevent excess movements at each joint
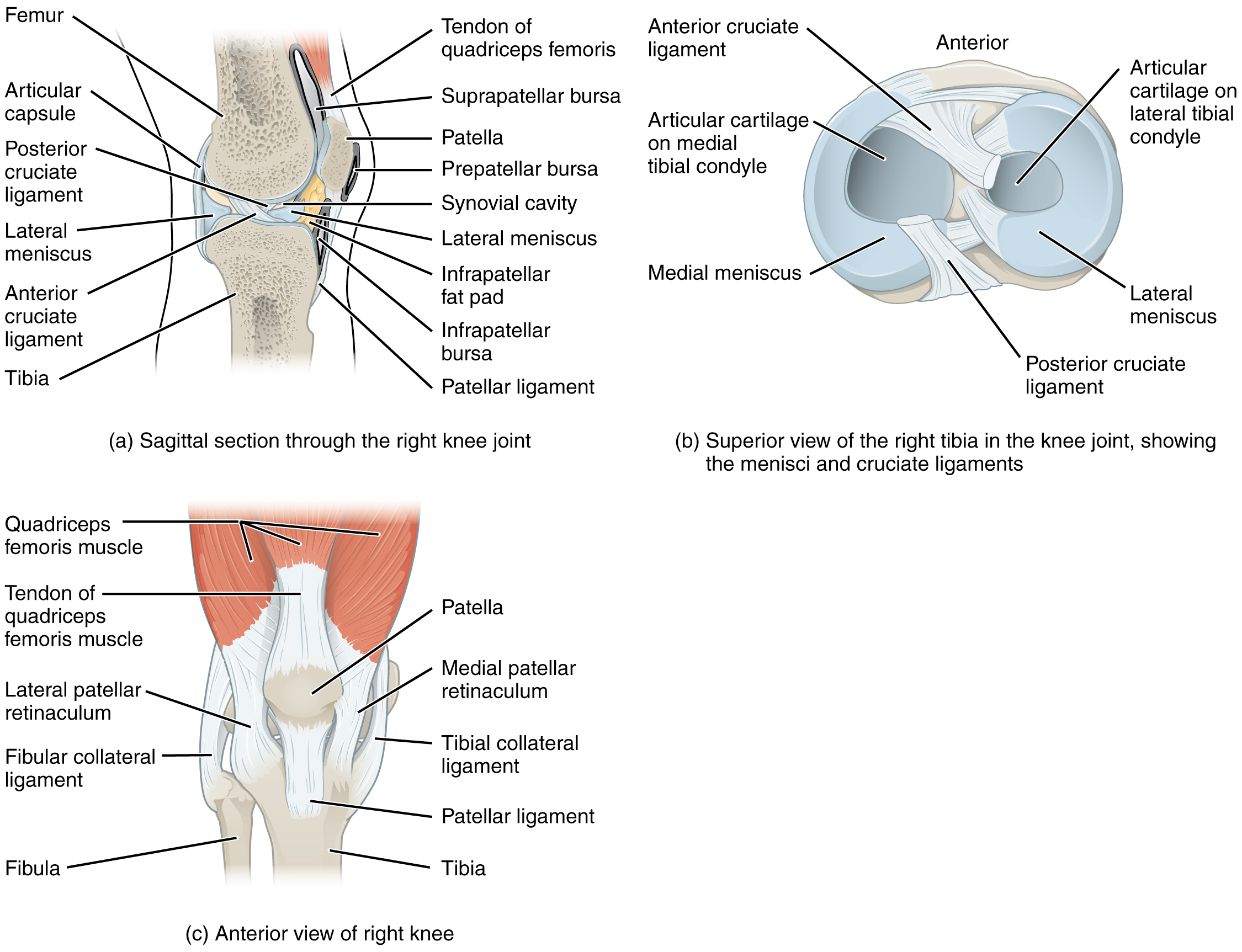
The knee joint is the largest joint of the body (Figure 9.19). It actually consists of three articulations. The femoropatellar joint is found between the patella and the distal femur. The medial tibiofemoral joint and lateral tibiofemoral joint are located between the medial and lateral condyles of the femur and the medial and lateral condyles of the tibia. All of these articulations are enclosed within a single articular capsule. The knee functions as a hinge joint, allowing flexion and extension of the leg. This action is generated by both rolling and gliding motions of the femur on the tibia. In addition, some rotation of the leg is available when the knee is flexed, but not when extended. The knee is well constructed for weight bearing in its extended position, but is vulnerable to injuries associated with hyperextension, twisting, or blows to the medial or lateral side of the joint, particularly while weight bearing.
At the femoropatellar joint, the patella slides vertically within a groove on the distal femur. The patella is a sesamoid bone incorporated into the tendon of the quadriceps femoris muscle, the large muscle of the anterior thigh. The patella serves to protect the quadriceps tendon from friction against the distal femur. Continuing from the patella to the anterior tibia just below the knee is the patellar ligament. Acting via the patella and patellar ligament, the quadriceps femoris is a powerful muscle that acts to extend the leg at the knee. It also serves as a “dynamic ligament” to provide very important support and stabilization for the knee joint.
The medial and lateral tibiofemoral joints are the articulations between the rounded condyles of the femur and the relatively flat condyles of the tibia. During flexion and extension motions, the condyles of the femur both roll and glide over the surfaces of the tibia. The rolling action produces flexion or extension, while the gliding action serves to maintain the femoral condyles centered over the tibial condyles, thus ensuring maximal bony, weight-bearing support for the femur in all knee positions. As the knee comes into full extension, the femur undergoes a slight medial rotation in relation to tibia. The rotation results because the lateral condyle of the femur is slightly smaller than the medial condyle. Thus, the lateral condyle finishes its rolling motion first, followed by the medial condyle. The resulting small medial rotation of the femur serves to “lock” the knee into its fully extended and most stable position. Flexion of the knee is initiated by a slight lateral rotation of the femur on the tibia, which “unlocks” the knee. This lateral rotation motion is produced by the popliteus muscle of the posterior leg.
Located between the articulating surfaces of the femur and tibia are two articular discs, the medial meniscus and lateral meniscus (see Figure 9.19b). Each is a C-shaped fibrocartilage structure that is thin along its inside margin and thick along the outer margin. They are attached to their tibial condyles, but do not attach to the femur. While both menisci are free to move during knee motions, the medial meniscus shows less movement because it is anchored at its outer margin to the articular capsule and tibial collateral ligament. The menisci provide padding between the bones and help to fill the gap between the round femoral condyles and flattened tibial condyles. Some areas of each meniscus lack an arterial blood supply and thus these areas heal poorly if damaged.
The knee joint has multiple ligaments that provide support, particularly in the extended position (see Figure 9.19c). Outside of the articular capsule, located at the sides of the knee, are two extrinsic ligaments. The fibular collateral ligament (lateral collateral ligament) is on the lateral side and spans from the lateral epicondyle of the femur to the head of the fibula. The tibial collateral ligament (medial collateral ligament) of the medial knee runs from the medial epicondyle of the femur to the medial tibia. As it crosses the knee, the tibial collateral ligament is firmly attached on its deep side to the articular capsule and to the medial meniscus, an important factor when considering knee injuries. In the fully extended knee position, both collateral ligaments are taut (tight), thus serving to stabilize and support the extended knee and preventing side-to-side or rotational motions between the femur and tibia.
The articular capsule of the posterior knee is thickened by intrinsic ligaments that help to resist knee hyperextension. Inside the knee are two intracapsular ligaments, the anterior cruciate ligament and posterior cruciate ligament. These ligaments are anchored inferiorly to the tibia at the intercondylar eminence, the roughened area between the tibial condyles. The cruciate ligaments are named for whether they are attached anteriorly or posteriorly to this tibial region. Each ligament runs diagonally upward to attach to the inner aspect of a femoral condyle. The cruciate ligaments are named for the X-shape formed as they pass each other (cruciate means “cross”). The posterior cruciate ligament is the stronger ligament. It serves to support the knee when it is flexed and weight bearing, as when walking downhill. In this position, the posterior cruciate ligament prevents the femur from sliding anteriorly off the top of the tibia. The anterior cruciate ligament becomes tight when the knee is extended, and thus resists hyperextension.
Figure 9.19 Knee Joint (a) The knee joint is the largest joint of the body. (b)–(c) It is supported by the tibial and fibular collateral ligaments located on the sides of the knee outside of the articular capsule, and the anterior and posterior cruciate ligaments found inside the capsule. The medial and lateral menisci provide padding and support between the femoral condyles and tibial condyles.
Interactive Link
Watch this video to learn more about the flexion and extension of the knee, as the femur both rolls and glides on the tibia to maintain stable contact between the bones in all knee positions. The patella glides along a groove on the anterior side of the distal femur. The collateral ligaments on the sides of the knee become tight in the fully extended position to help stabilize the knee. The posterior cruciate ligament supports the knee when flexed and the anterior cruciate ligament becomes tight when the knee comes into full extension to resist hyperextension. What are the ligaments that support the knee joint?
Interactive Link
Watch this video to learn more about the anatomy of the knee joint, including bones, joints, muscles, nerves, and blood vessels. Which ligament of the knee keeps the tibia from sliding too far forward in relation to the femur and which ligament keeps the tibia from sliding too far backward?
Disorders of the…Joints
Injuries to the knee are common. Since this joint is primarily supported by muscles and ligaments, injuries to any of these structures will result in pain or knee instability. Injury to the posterior cruciate ligament occurs when the knee is flexed and the tibia is driven posteriorly, such as falling and landing on the tibial tuberosity or hitting the tibia on the dashboard when not wearing a seatbelt during an automobile accident. More commonly, injuries occur when forces are applied to the extended knee, particularly when the foot is planted and unable to move. Anterior cruciate ligament injuries can result with a forceful blow to the anterior knee, producing hyperextension, or when a runner makes a quick change of direction that produces both twisting and hyperextension of the knee.
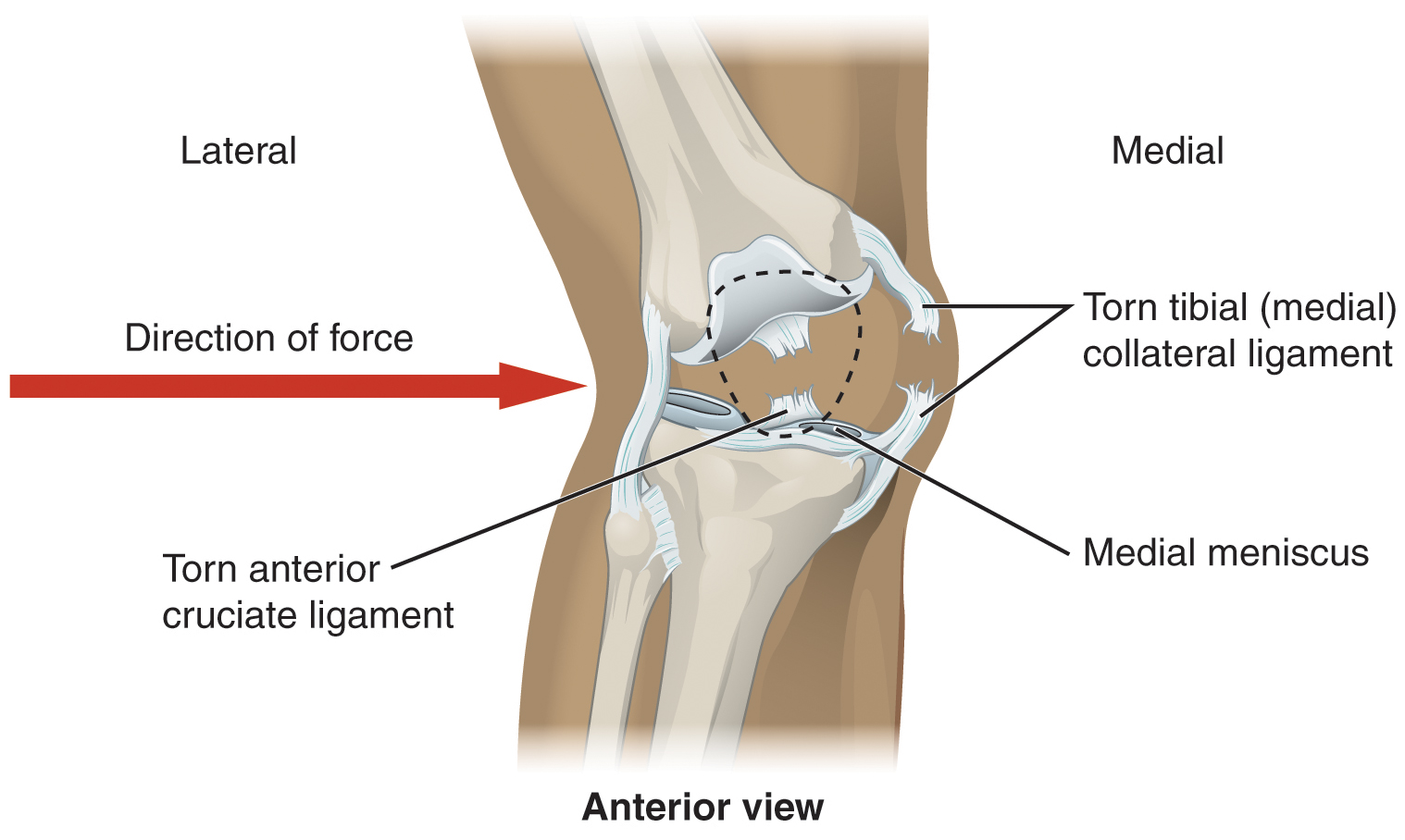
A worse combination of injuries can occur with a hit to the lateral side of the extended knee (Figure 9.20). A moderate blow to the lateral knee will cause the medial side of the joint to open, resulting in stretching or damage to the tibial collateral ligament. Because the medial meniscus is attached to the tibial collateral ligament, a stronger blow can tear the ligament and also damage the medial meniscus. This is one reason that the medial meniscus is 20 times more likely to be injured than the lateral meniscus. A powerful blow to the lateral knee produces a “terrible triad” injury, in which there is a sequential injury to the tibial collateral ligament, medial meniscus, and anterior cruciate ligament.
Arthroscopic surgery has greatly improved the surgical treatment of knee injuries and reduced subsequent recovery times. This procedure involves a small incision and the insertion into the joint of an arthroscope, a pencil-thin instrument that allows for visualization of the joint interior. Small surgical instruments are also inserted via additional incisions. These tools allow a surgeon to remove or repair a torn meniscus or to reconstruct a ruptured cruciate ligament. The current method for anterior cruciate ligament replacement involves using a portion of the patellar ligament. Holes are drilled into the cruciate ligament attachment points on the tibia and femur, and the patellar ligament graft, with small areas of attached bone still intact at each end, is inserted into these holes. The bone-to-bone sites at each end of the graft heal rapidly and strongly, thus enabling a rapid recovery.
Figure 9.20 Knee Injury A strong blow to the lateral side of the extended knee will cause three injuries, in sequence: tearing of the tibial collateral ligament, damage to the medial meniscus, and rupture of the anterior cruciate ligament.
Interactive Link
Watch this video to learn more about different knee injuries and diagnostic testing of the knee. What are the most common causes of anterior cruciate ligament injury?\
Chapter Review
Classification of Joints
Structural classifications of the body joints are based on how the bones are held together and articulate with each other. At fibrous joints, the adjacent bones are directly united to each other by fibrous connective tissue. Similarly, at a cartilaginous joint, the adjacent bones are united by cartilage. In contrast, at a synovial joint, the articulating bone surfaces are not directly united to each other, but come together within a fluid-filled joint cavity.
The functional classification of body joints is based on the degree of movement found at each joint. A synarthrosis is a joint that is essentially immobile. This type of joint provides for a strong connection between the adjacent bones, which serves to protect internal structures such as the brain or heart. Examples include the fibrous joints of the skull sutures and the cartilaginous manubriosternal joint. A joint that allows for limited movement is an amphiarthrosis. An example is the pubic symphysis of the pelvis, the cartilaginous joint that strongly unites the right and left hip bones of the pelvis. The cartilaginous joints in which vertebrae are united by intervertebral discs provide for small movements between the adjacent vertebrae and are also an amphiarthrosis type of joint. Thus, based on their movement ability, both fibrous and cartilaginous joints are functionally classified as a synarthrosis or amphiarthrosis.
The most common type of joint is the diarthrosis, which is a freely moveable joint. All synovial joints are functionally classified as diarthroses. A uniaxial diarthrosis, such as the elbow, is a joint that only allows for movement within a single anatomical plane. Joints that allow for movements in two planes are biaxial joints, such as the metacarpophalangeal joints of the fingers. A multiaxial joint, such as the shoulder or hip joint, allows for three planes of motions.
Fibrous Joints
Fibrous joints are where adjacent bones are strongly united by fibrous connective tissue. The gap filled by connective tissue may be narrow or wide. The three types of fibrous joints are sutures, gomphoses, and syndesmoses. A suture is the narrow fibrous joint that unites most bones of the skull. At a gomphosis, the root of a tooth is anchored across a narrow gap by periodontal ligaments to the walls of its socket in the bony jaw. A syndesmosis is the type of fibrous joint found between parallel bones. The gap between the bones may be wide and filled with a fibrous interosseous membrane, or it may narrow with ligaments spanning between the bones. Syndesmoses are found between the bones of the forearm (radius and ulna) and the leg (tibia and fibula). Fibrous joints strongly unite adjacent bones and thus serve to provide protection for internal organs, strength to body regions, or weight-bearing stability.
Cartilaginous Joints
There are two types of cartilaginous joints. A synchondrosis is formed when the adjacent bones are united by hyaline cartilage. A temporary synchondrosis is formed by the epiphyseal plate of a growing long bone, which is lost when the epiphyseal plate ossifies as the bone reaches maturity. The synchondrosis is thus replaced by a synostosis. Permanent synchondroses that do not ossify are found at the first sternocostal joint and between the anterior ends of the bony ribs and the junction with their costal cartilage. A symphysis is where the bones are joined by fibrocartilage and the gap between the bones may be narrow or wide. A narrow symphysis is found at the manubriosternal joint and at the pubic symphysis. A wide symphysis is the intervertebral symphysis in which the bodies of adjacent vertebrae are united by an intervertebral disc.
Synovial Joints
Synovial joints are the most common type of joints in the body. They are characterized by the presence of a joint cavity, inside of which the bones of the joint articulate with each other. The articulating surfaces of the bones at a synovial joint are not directly connected to each other by connective tissue or cartilage, which allows the bones to move freely against each other. The walls of the joint cavity are formed by the articular capsule. Friction between the bones is reduced by a thin layer of articular cartilage covering the surfaces of the bones, and by a lubricating synovial fluid, which is secreted by the synovial membrane.
Synovial joints are strengthened by the presence of ligaments, which hold the bones together and resist excessive or abnormal movements of the joint. Ligaments are classified as extrinsic ligaments if they are located outside of the articular capsule, intrinsic ligaments if they are fused to the wall of the articular capsule, or intracapsular ligaments if they are located inside the articular capsule. Some synovial joints also have an articular disc (meniscus), which can provide padding between the bones, smooth their movements, or strongly join the bones together to strengthen the joint. Muscles and their tendons acting across a joint can also increase their contractile strength when needed, thus providing indirect support for the joint.
Anatomy of the Knee Joint
Although synovial joints share many common features, each joint of the body is specialized for certain movements and activities. The joints of the upper limb provide for large ranges of motion, which give the upper limb great mobility, thus enabling actions such as the throwing of a ball or typing on a keyboard. The joints of the lower limb are more robust, giving them greater strength and the stability needed to support the body weight during running, jumping, or kicking activities.
The knee includes three articulations. The femoropatellar joint is between the patella and distal femur. The patella, a sesamoid bone incorporated into the tendon of the quadriceps femoris muscle of the anterior thigh, serves to protect this tendon from rubbing against the distal femur during knee movements. The medial and lateral tibiofemoral joints, between the condyles of the femur and condyles of the tibia, are modified hinge joints that allow for knee extension and flexion. During these movements, the condyles of the femur both roll and glide over the surface of the tibia. As the knee comes into full extension, a slight medial rotation of the femur serves to “lock” the knee into its most stable, weight-bearing position. The reverse motion, a small lateral rotation of the femur, is required to initiate knee flexion. When the knee is flexed, some rotation of the leg is available.
Two extrinsic ligaments, the tibial collateral ligament on the medial side and the fibular collateral ligament on the lateral side, serve to resist hyperextension or rotation of the extended knee joint. Two intracapsular ligaments, the anterior cruciate ligament and posterior cruciate ligament, span between the tibia and the inner aspects of the femoral condyles. The anterior cruciate ligament resists hyperextension of the knee, while the posterior cruciate ligament prevents anterior sliding of the femur, thus supporting the knee when it is flexed and weight bearing. The medial and lateral menisci, located between the femoral and tibial condyles, are articular discs that provide padding and improve the fit between the bones.
Critical Thinking Questions
Explain the reasons for why joints differ in their degree of mobility.
Describe the two types of cartilaginous joints and give examples of each.
Describe the characteristic structures found at all synovial joints.
Describe the structures that provide direct and indirect support for a synovial joint.
Describe the sequence of injuries that may occur if the extended, weight-bearing knee receives a very strong blow to the lateral side of the knee.