Human Body Tissues
Introduction to Tissues
Learning Objectives
By the end of this section, you will be able to:
- Identify the four main tissue types
- Discuss the functions of each tissue type
- Relate the structure of each tissue type to their function
The term tissue is used to describe a group of cells found together in the body. The cells within a tissue share a common embryonic origin. Microscopic observation reveals that the cells in a tissue share morphological features and are arranged in an orderly pattern that achieves the tissue’s functions. From the evolutionary perspective, tissues appear in more complex organisms. For example, multicellular protists, ancient eukaryotes, do not have cells organized into tissues.
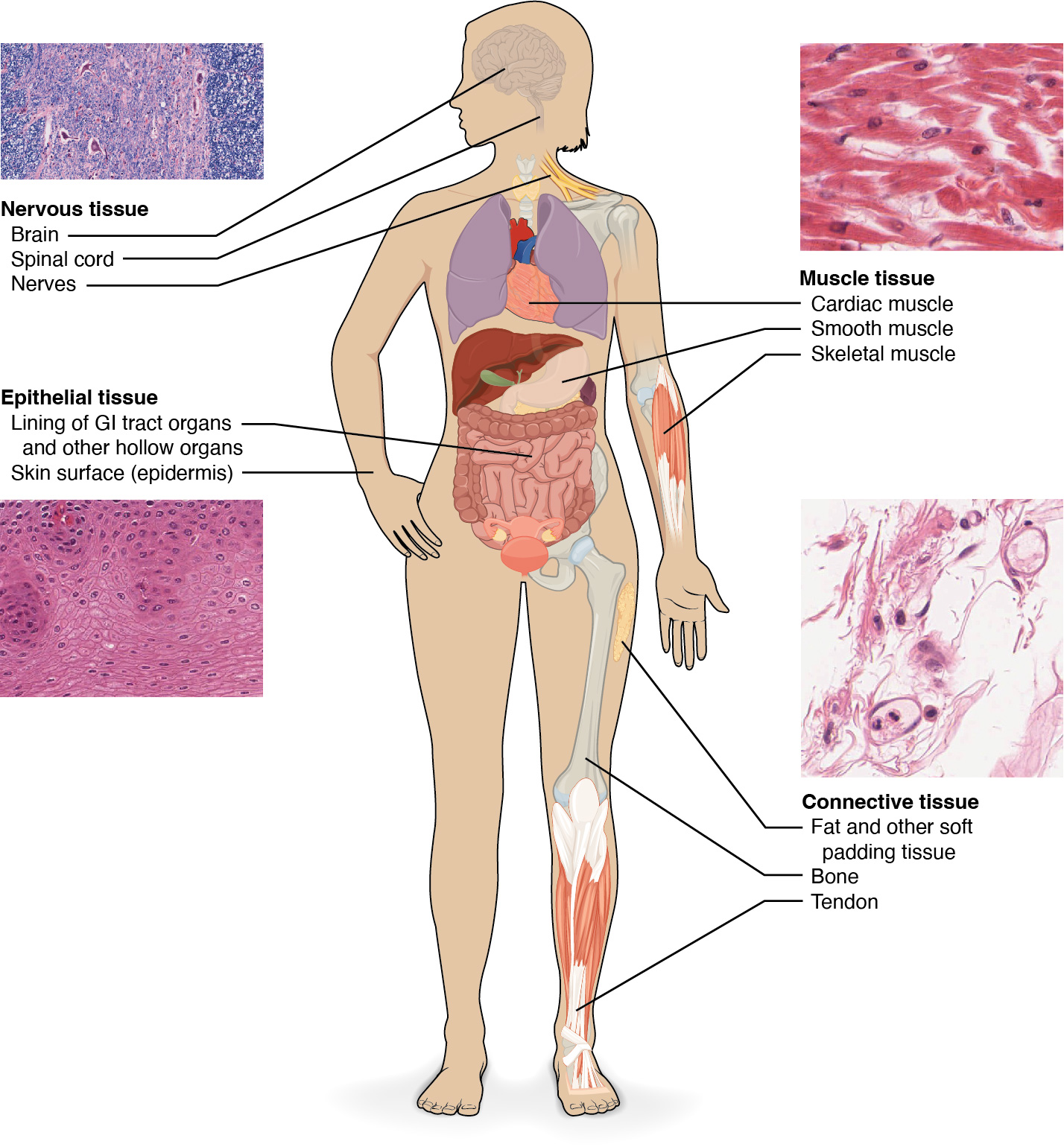
Although there are many types of cells in the human body, they are organized into four broad categories of tissues: epithelial, connective, muscle, and nervous. Each of these categories is characterized by specific functions that contribute to the overall health and maintenance of the body. A disruption of the structure is a sign of injury or disease. Such changes can be detected through histology, the microscopic study of tissue appearance, organization, and function.
Epithelial tissue, also referred to as epithelium, refers to the sheets of cells that cover exterior surfaces of the body, line internal cavities and passageways, and form certain glands. Connective tissue, as its name implies, binds the cells and organs of the body together and functions in the protection, support, and integration of all parts of the body. Muscle tissue is excitable, responding to stimulation and contracting to provide movement, and occurs as three major types: skeletal (voluntary) muscle, smooth muscle, and cardiac muscle in the heart. Nervous tissue is also excitable, allowing the propagation of electrochemical signals in the form of nerve impulses that communicate between different regions of the body (Figure 4.2).
The next level of organization is the organ, where several types of tissues come together to form a working unit. Just as knowing the structure and function of cells helps you in your study of tissues, knowledge of tissues will help you understand how organs function. The epithelial and connective tissues are discussed in detail in this chapter. Muscle and nervous tissues will be discussed only briefly in this chapter.
Figure 4.2 Four Types of Tissue: Body The four types of tissues are exemplified in nervous tissue, stratified squamous epithelial tissue, cardiac muscle tissue, and connective tissue. (Micrographs provided by the Regents of University of Michigan Medical School © 2012)
Cell to Cell Junctions
Learning Objectives
By the end of this section, you will be able to:
- Distinguish between tight junctions, desmosomes (anchoring junctions), and gap junctions
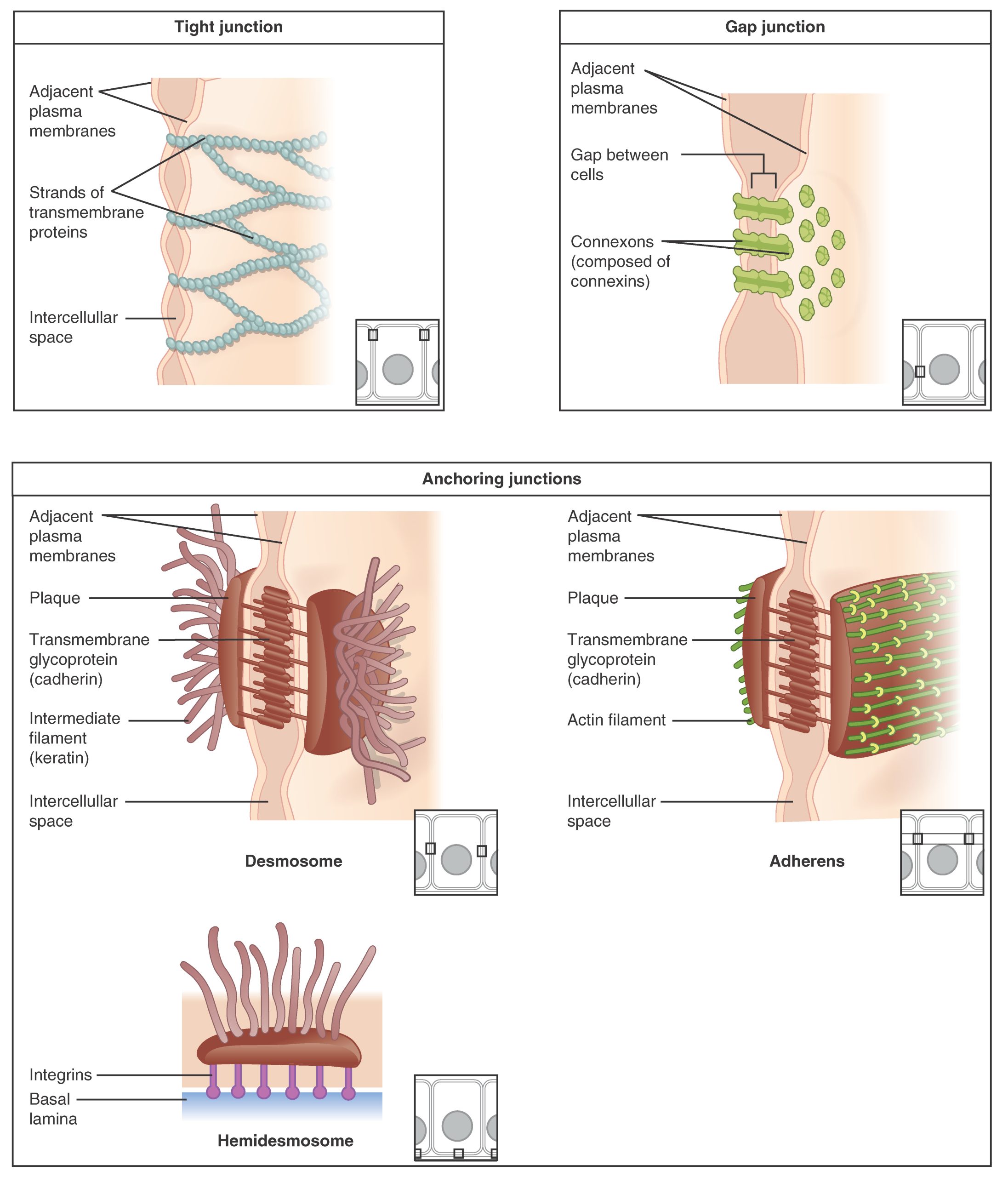
In some tissues, the cells are held together by different types of junctions as a tissue. Other tissues, the cells are surrounded by extracellular substances so the cells are not ‘attached’ to each other. There are three basic types of connections allow varying degrees of interaction between the cells: tight junctions, desmosomes (anchoring junctions), and gap junctions (Figure 4.5).
Figure 4.5 Types of Cell Junctions The three basic types of cell-to-cell junctions are tight junctions, gap junctions, and anchoring junctions.
At one end of the spectrum is the tight junction, which separates the cells into apical and basal compartments. When two adjacent epithelial cells form a tight junction, there is no extracellular space between them and the movement of substances through the extracellular space between the cells is blocked. This enables the epithelia to act as selective barriers.
An anchoring junctions or desmosomes includes several types of cell junctions that help stabilize epithelial tissues. Anchoring junctions are common on the lateral and basal surfaces of cells where they provide strong and flexible connections. The junctions are characterized by the presence of the contractile protein actin located on the cytoplasmic surface of the cell membrane. The actin can connect isolated patches or form a belt-like structure inside the cell. These junctions influence the shape and folding of the epithelial tissue.
In contrast with the tight and anchoring junctions, a gap junction forms an intercellular passageway between the membranes of adjacent cells to facilitate the movement of small molecules and ions between the cytoplasm of adjacent cells. These junctions allow electrical and metabolic coupling of adjacent cells, which coordinates function in large groups of cells.
Epithelial Tissue
Learning Objectives
By the end of this section, you will be able to:
- Explain the structure and function of epithelial tissue
- Distinguish between simple epithelia and stratified epithelia, as well as between squamous, cuboidal, and columnar epithelia
Most epithelial tissues are essentially large sheets of cells covering all the surfaces of the body exposed to the outside world and lining the outside of organs. Epithelium also forms much of the glandular tissue of the body. Skin is not the only area of the body exposed to the outside. Other areas include the airways, the digestive tract, as well as the urinary and reproductive systems, all of which are lined by an epithelium. Hollow organs and body cavities that do not connect to the exterior of the body, which includes, blood vessels and serous membranes, are lined by endothelium (plural = endothelia), which is a type of epithelium.
All epithelia share some important structural and functional features. This tissue is highly cellular, with little or no extracellular material present between cells. Adjoining cells form a specialized intercellular connection between their cell membranes called a cell junction. The epithelial cells exhibit polarity with differences in structure and function between the exposed or apical facing surface of the cell and the basal surface close to the underlying body structures. The basal lamina, a mixture of glycoproteins and collagen, provides an attachment site for the epithelium, separating it from underlying connective tissue. The basal lamina attaches to a reticular lamina, which is secreted by the underlying connective tissue, forming a basement membrane that helps hold it all together.
Epithelial tissues are nearly completely avascular. For instance, no blood vessels cross the basement membrane to enter the tissue, and nutrients must come by diffusion or absorption from underlying tissues or the surface. Many epithelial tissues are capable of rapidly replacing damaged and dead cells. Sloughing off of damaged or dead cells is a characteristic of surface epithelium and allows our airways and digestive tracts to rapidly replace damaged cells with new cells.
Generalized Functions of Epithelial Tissue
Epithelial tissues provide the body’s first line of protection from physical, chemical, and biological wear and tear. The cells of an epithelium act as gatekeepers of the body controlling permeability and allowing selective transfer of materials across a physical barrier. All substances that enter the body must cross an epithelium. Some epithelia often include structural features that allow the selective transport of molecules and ions across their cell membranes.
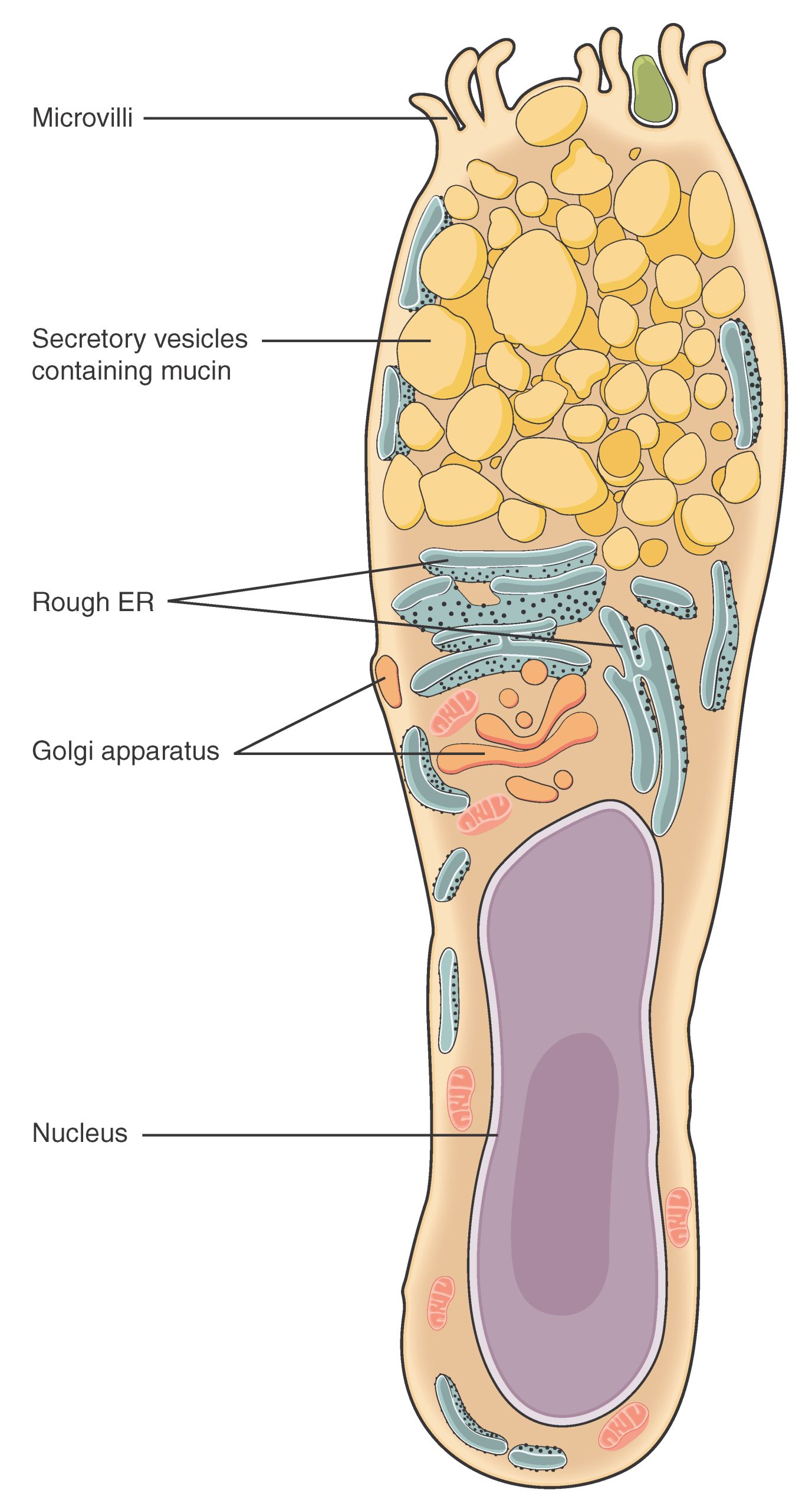
Many epithelial cells are capable of secretion and release mucous and specific chemical compounds onto their apical surfaces. The epithelium of the small intestine releases digestive enzymes, for example. Cells lining the respiratory tract secrete mucous that traps incoming microorganisms and particles. A glandular epithelium contains many secretory cells.
The Epithelial Cell
Epithelial cells are typically characterized by the polarized distribution of organelles and membrane-bound proteins between their basal and apical surfaces. Particular structures found in some epithelial cells are an adaptation to specific functions. Certain organelles are segregated to the basal sides, whereas other organelles and extensions, such as cilia, when present, are on the apical surface.
Cilia are microscopic extensions of the apical cell membrane that are supported by proteins (microtubules). They beat in unison and move fluids as well as trapped particles. Ciliated epithelium lines the ventricles of the brain where it helps circulate the cerebrospinal fluid. The ciliated epithelium of your airway forms a mucociliary escalator that sweeps particles of dust and pathogens trapped in the secreted mucous toward the throat. It is called an escalator because it continuously pushes mucous with trapped particles upward. In contrast, nasal cilia sweep the mucous blanket down towards your throat. In both cases, the transported materials are usually swallowed, and end up in the acidic environment of your stomach.
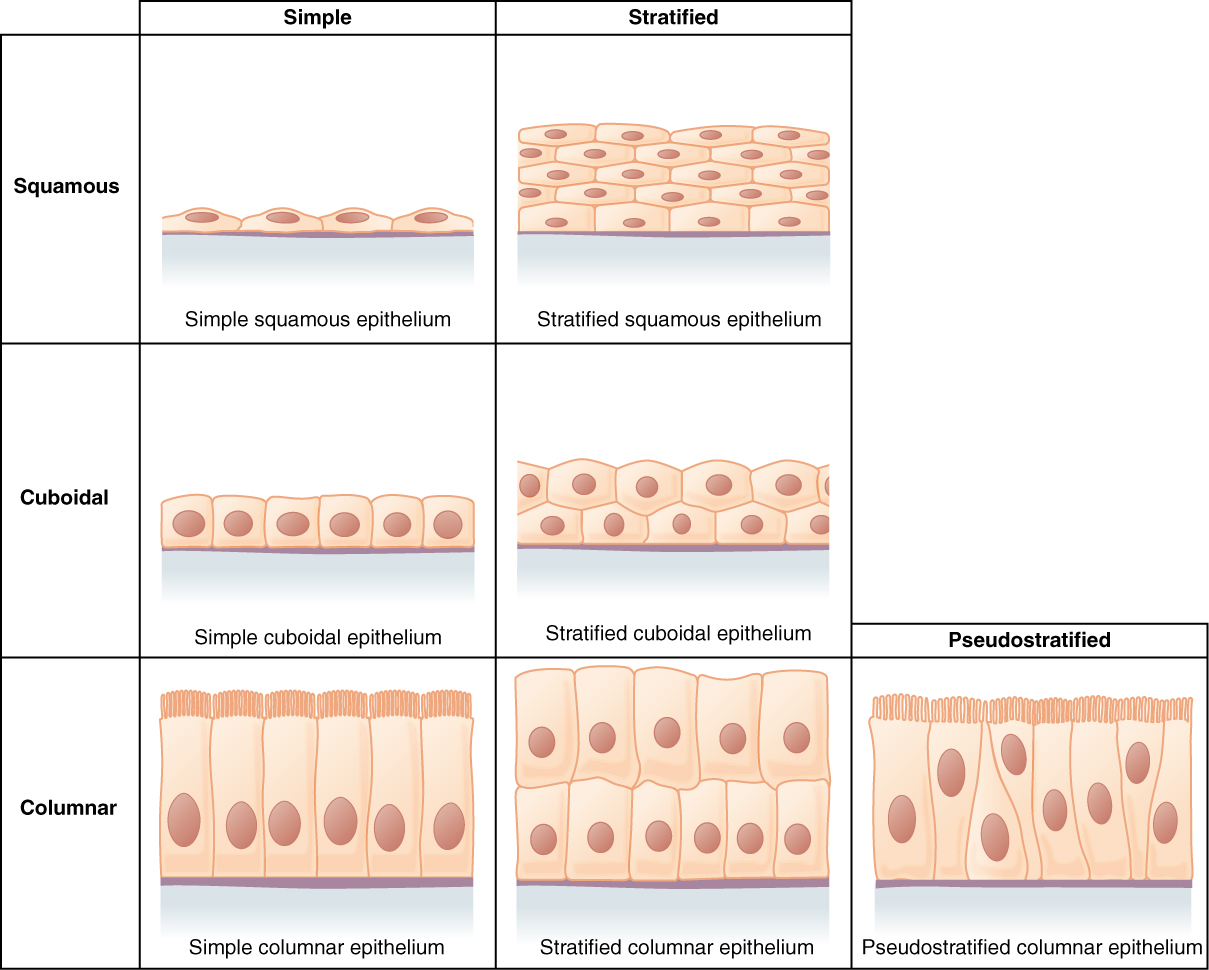
Classification of Epithelial Tissues
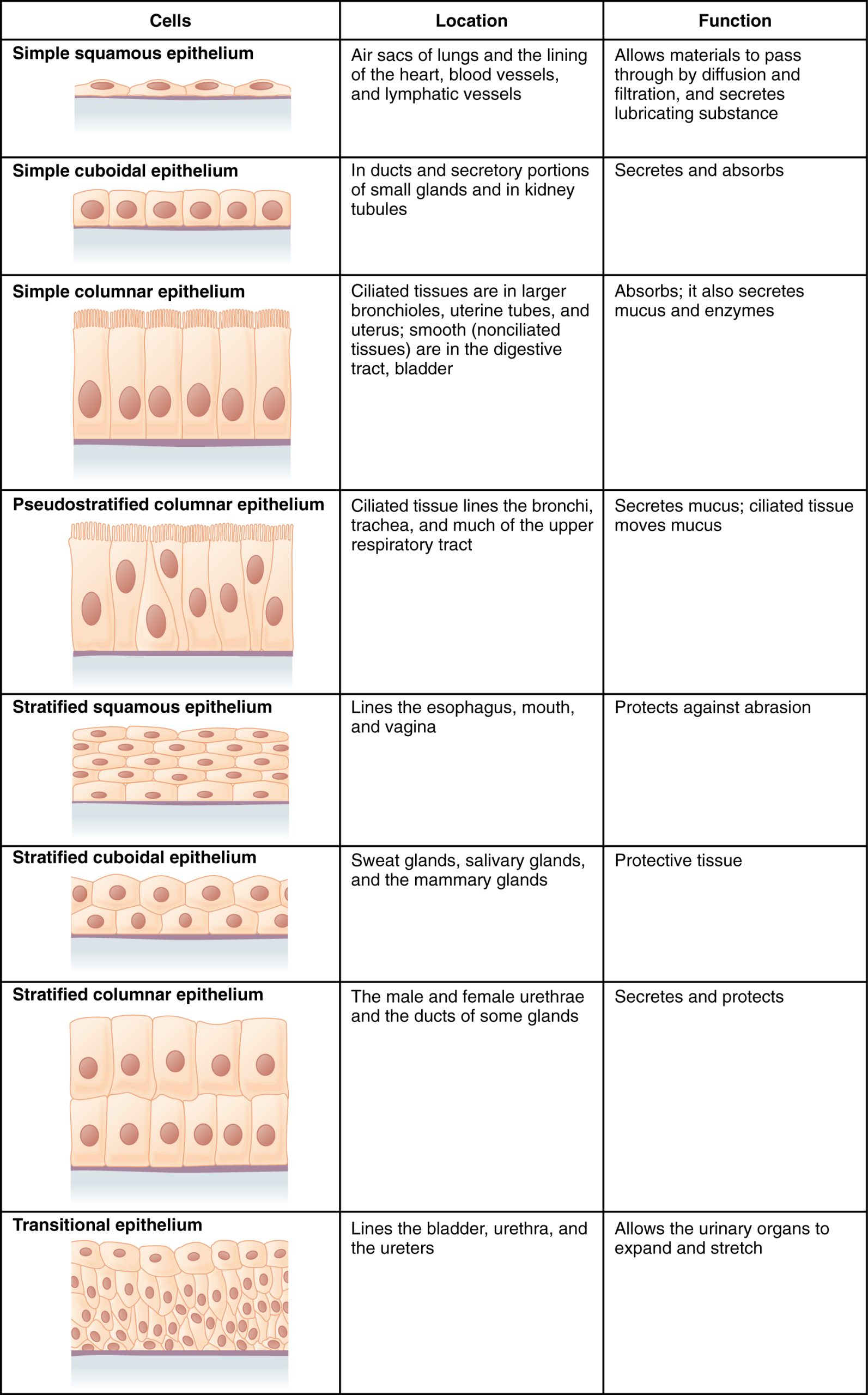
Epithelial tissues are classified according to the shape of the cells and number of the cell layers formed (Figure 4.6). Cell shapes can be squamous (flattened and thin), cuboidal (boxy, as wide as it is tall), or columnar (rectangular, taller than it is wide). Similarly, the number of cell layers in the tissue can be one—where every cell rests on the basal lamina—which is a simple epithelium, or more than one, which is a stratified epithelium and only the basal layer of cells rests on the basal lamina. Pseudostratified (pseudo- = “false”) describes tissue with a single layer of irregularly shaped cells that give the appearance of more than one layer. Transitional describes a form of specialized stratified epithelium in which the shape of the cells can vary.
Figure 4.6 Cells of Epithelial Tissue Simple epithelial tissue is organized as a single layer of cells and stratified epithelial tissue is formed by several layers of cells.
Simple Epithelium
The shape of the cells in the single cell layer of simple epithelium reflects the functioning of those cells. The cells in simple squamous epithelium have the appearance of thin scales. Squamous cell nuclei tend to be flat, horizontal, and elliptical, mirroring the form of the cell. The endothelium is the epithelial tissue that lines vessels of the lymphatic and cardiovascular system, and it is made up of a single layer of squamous cells. Simple squamous epithelium, because of the thinness of the cell, is present where rapid passage of chemical compounds is observed. The alveoli of lungs where gases diffuse, segments of kidney tubules, and the lining of capillaries are also made of simple squamous epithelial tissue. The mesothelium is a simple squamous epithelium that forms the surface layer of the serous membrane that lines body cavities and internal organs. Its primary function is to provide a smooth and protective surface. Mesothelial cells are squamous epithelial cells that secrete a fluid that lubricates the mesothelium.
In simple cuboidal epithelium, the nucleus of the box-like cells appears round and is generally located near the center of the cell. These epithelia are active in the secretion and absorptions of molecules. Simple cuboidal epithelia are observed in the lining of the kidney tubules and in the ducts of glands.
In simple columnar epithelium, the nucleus of the tall column-like cells tends to be elongated and located in the basal end of the cells. Like the cuboidal epithelia, this epithelium is active in the absorption and secretion of molecules. Simple columnar epithelium forms the lining of some sections of the digestive system and parts of the female reproductive tract. Ciliated columnar epithelium is composed of simple columnar epithelial cells with cilia on their apical surfaces. These epithelial cells are found in the lining of the fallopian tubes and parts of the respiratory system, where the beating of the cilia helps remove particulate matter.
Pseudostratified columnar epithelium is a type of epithelium that appears to be stratified but instead consists of a single layer of irregularly shaped and differently sized columnar cells. In pseudostratified epithelium, nuclei of neighboring cells appear at different levels rather than clustered in the basal end. The arrangement gives the appearance of stratification; but in fact all the cells are in contact with the basal lamina, although some do not reach the apical surface. Pseudostratified columnar epithelium is found in the respiratory tract, where some of these cells have cilia.
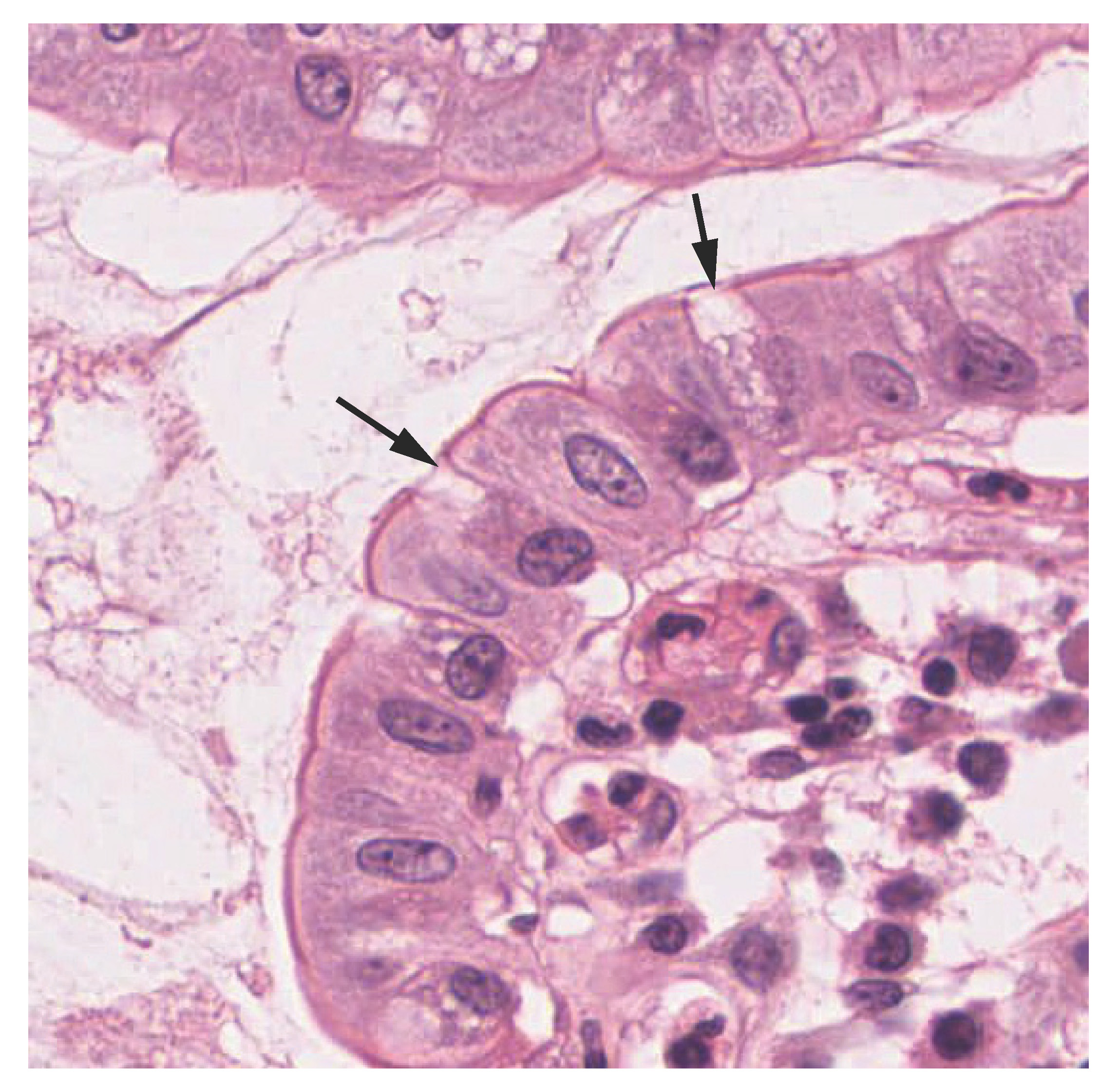
Both simple and pseudostratified columnar epithelia are heterogeneous epithelia because they include additional types of cells interspersed among the epithelial cells. For example, a goblet cell is a mucous-secreting unicellular “gland” interspersed between the columnar epithelial cells of mucous membranes (Figure 4.7).
Figure 4.7 Goblet Cell (a) In the lining of the small intestine, columnar epithelium cells are interspersed with goblet cells. (b) The arrows in this micrograph point to the mucous-secreting goblet cells. LM × 1600. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Interactive Link
View the University of Michigan WebScope to explore the tissue sample in greater detail.
Stratified Epithelium
A stratified epithelium consists of several stacked layers of cells. This epithelium protects against physical and chemical wear and tear. The stratified epithelium is named by the shape of the most apical layer of cells, closest to the free space. Stratified squamous epithelium is the most common type of stratified epithelium in the human body. The apical cells are squamous, whereas the basal layer contains either columnar or cuboidal cells. The top layer may be covered with dead cells filled with keratin. Mammalian skin is an example of this dry, keratinized, stratified squamous epithelium. The lining of the mouth cavity is an example of an unkeratinized, stratified squamous epithelium. Stratified cuboidal epithelium and stratified columnar epithelium can also be found in certain glands and ducts, but are uncommon in the human body.
Another kind of stratified epithelium is transitional epithelium, so-called because of the gradual changes in the shapes of the apical cells as the bladder fills with urine. It is found only in the urinary system, specifically the ureters and urinary bladder. When the bladder is empty, this epithelium is convoluted and has cuboidal apical cells with convex, umbrella shaped, apical surfaces. As the bladder fills with urine, this epithelium loses its convolutions and the apical cells transition from cuboidal to squamous. It appears thicker and more multi-layered when the bladder is empty, and more stretched out and less stratified when the bladder is full and distended. Figure 4.8 summarizes the different categories of epithelial cell tissue cells.
Figure 4.8 Summary of Epithelial Tissue Cells
Interactive Link
Watch this video to find out more about the anatomy of epithelial tissues. Where in the body would one find non-keratinizing stratified squamous epithelium?
Glandular Epithelium
Learning Objectives
By the end of this section, you will be able to:
- Describe the structure and function of endocrine and exocrine glands and their respective secretions
A gland is a structure made up of one or more cells modified to synthesize and secrete chemical substances. Most glands consist of groups of epithelial cells. A gland can be classified as an endocrine gland, a ductless gland that releases secretions directly into surrounding tissues and fluids (endo- = “inside”), or an exocrine gland whose secretions leave through a duct that opens directly, or indirectly, to the external environment (exo- = “outside”).
Endocrine Glands
The secretions of endocrine glands are called hormones. Hormones are released into the interstitial fluid, diffused into the bloodstream, and delivered to targets, in other words, cells that have receptors to bind the hormones. The endocrine system is part of a major regulatory system coordinating the regulation and integration of body responses. A few examples of endocrine glands include the pituitary gland, thymus gland, adrenal gland, and gonads (testes and ovaries).
Exocrine Glands
Exocrine glands release their contents through a duct that leads to the epithelial surface. Mucous, sweat, saliva, and breast milk are all examples of secretions from exocrine glands. They are all discharged through tubular ducts. Secretions into the lumen of the gastrointestinal tract, technically outside of the body, are of the exocrine category.
Connective Tissue
Learning Objectives
By the end of this section, you will be able to:
- Identify and distinguish between the types of connective tissue
- Explain the functions of connective tissues
As may be obvious from its name, one of the major functions of connective tissue is to connect tissues and organs. Unlike epithelial tissue, which is composed of cells closely packed with little or no extracellular space in between, connective tissue cells are dispersed in a matrix. The matrix usually includes a large amount of extracellular material produced by the connective tissue cells that are embedded within it. The matrix plays a major role in the functioning of this tissue. The major component of the matrix is a ground substance often crisscrossed by protein fibers. This ground substance is usually a fluid, but it can also be mineralized and solid, as in bones. Connective tissues come in a vast variety of forms, yet they typically have in common three characteristic components: cells, large amounts of amorphous ground substance, and protein fibers. The amount and structure of each component correlates with the function of the tissue, from the rigid ground substance in bones supporting the body to the inclusion of specialized cells; for example, a phagocytic cell that engulfs pathogens and also rids tissue of cellular debris.
Functions of Connective Tissues
Connective tissues perform many functions in the body, but most importantly, they support and connect other tissues; from the connective tissue sheath that surrounds muscle cells, to the tendons that attach muscles to bones, and to the skeleton that supports the positions of the body. Protection is another major function of connective tissue, in the form of fibrous capsules and bones that protect delicate organs and, of course, the skeletal system. Specialized cells in connective tissue defend the body from microorganisms that enter the body. Transport of fluid, nutrients, waste, and chemical messengers is ensured by specialized fluid connective tissues, such as blood and lymph. Adipose cells store surplus energy in the form of fat and contribute to the thermal insulation of the body.
Classification of Connective Tissues
The three broad categories of connective tissue are classified according to the characteristics of their ground substance and the types of fibers found within the matrix (Table 4.1). Connective tissue proper includes loose connective tissue and dense connective tissue. Both tissues have a variety of cell types and protein fibers suspended in a viscous ground substance. Dense connective tissue is reinforced by bundles of fibers that provide tensile strength, elasticity, and protection. In loose connective tissue, the fibers are loosely organized, leaving large spaces in between. Supportive connective tissue—bone and cartilage—provide structure and strength to the body and protect soft tissues. A few distinct cell types and densely packed fibers in a matrix characterize these tissues. In bone, the matrix is rigid and described as calcified because of the deposited calcium salts. In fluid connective tissue, in other words, lymph and blood, various specialized cells circulate in a watery fluid containing salts, nutrients, and dissolved proteins.
|
Connective tissue proper |
Supportive connective tissue |
Fluid connective tissue |
|
Areolar Adipose Reticular Dense Fibrous
|
Hyaline Cartilage Fibrocartilage Elastic Cartilage Bone |
Blood
|
Table 4.1 Connective Tissue Examples
Connective Tissue Proper
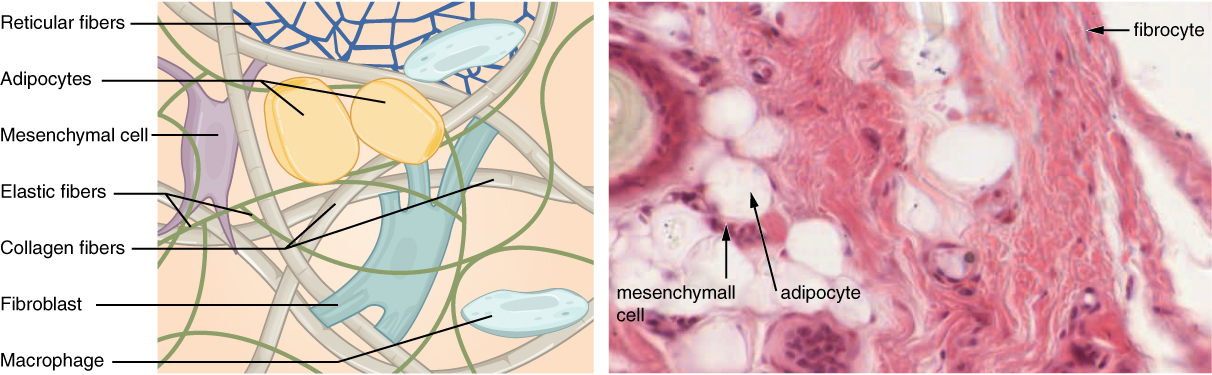
Fibroblasts are present in all connective tissue proper (Figure 4.12). Fibrocytes, adipocytes, and mesenchymal cells are fixed cells, which means they remain within the connective tissue. Other cells move in and out of the connective tissue in response to chemical signals. Macrophages, mast cells, lymphocytes, plasma cells, and phagocytic cells are found in connective tissue proper but are actually part of the immune system protecting the body.
Figure 4.12 Connective Tissue Proper Fibroblasts produce this fibrous tissue. Connective tissue proper includes the fixed cells fibrocytes, adipocytes, and mesenchymal cells. LM × 400. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Cell Types
The most abundant cell in connective tissue proper is the fibroblast. Polysaccharides and proteins secreted by fibroblasts combine with extra-cellular fluids to produce a viscous ground substance that, with embedded fibrous proteins, forms the extra-cellular matrix. As you might expect, a fibrocyte, a less active form of fibroblast, is the second most common cell type in connective tissue proper.
Adipocytes are cells that store lipids as droplets that fill most of the cytoplasm. There are two basic types of adipocytes: white and brown. The brown adipocytes store lipids as many droplets, and have high metabolic activity. In contrast, white fat adipocytes store lipids as a single large drop and are metabolically less active. Their effectiveness at storing large amounts of fat is witnessed in obese individuals. The number and type of adipocytes depends on the tissue and location, and vary among individuals in the population.
The macrophage cell is a large cell derived from a monocyte, a type of blood cell, which enters the connective tissue matrix from the blood vessels. The macrophage cells are an essential component of the immune system, which is the body’s defense against potential pathogens and degraded host cells. When stimulated, macrophages release cytokines, small proteins that act as chemical messengers. Cytokines recruit other cells of the immune system to infected sites and stimulate their activities. Roaming, or free, macrophages move rapidly by amoeboid movement, engulfing infectious agents and cellular debris. In contrast, fixed macrophages are permanent residents of their tissues.
The mast cell, found in connective tissue proper, has many cytoplasmic granules. These granules contain the chemical signals histamine and heparin. When irritated or damaged, mast cells release histamine, an inflammatory mediator, which causes vasodilation and increased blood flow at a site of injury or infection, along with itching, swelling, and redness you recognize as an allergic response.
Connective Tissue Fibers and Ground Substance
Three main types of fibers are secreted by fibroblasts: collagen fibers, elastic fibers, and reticular fibers. Collagen fiber is made from fibrous protein subunits linked together to form a long and straight fiber. Collagen fibers, while flexible, have great tensile strength, resist stretching, and give ligaments and tendons their characteristic resilience and strength. These fibers hold connective tissues together, even during the movement of the body.
Elastic fiber contains the protein elastin along with lesser amounts of other proteins and glycoproteins. The main property of elastin is that after being stretched or compressed, it will return to its original shape. Elastic fibers are prominent in elastic tissues found in skin and the elastic ligaments of the vertebral column.
Reticular fiber is also formed from the same protein subunits as collagen fibers; however, these fibers remain narrow and are arrayed in a branching network. They are found throughout the body, but are most abundant in the reticular tissue of soft organs, such as liver and spleen, where they anchor and provide structural support to the parenchyma (the functional cells, blood vessels, and nerves of the organ).
All of these fiber types are embedded in ground substance. Secreted by fibroblasts, ground substance is made of polysaccharides, specifically hyaluronic acid, and proteins. These combine to form a proteoglycan with a protein core and polysaccharide branches. The proteoglycan attracts and traps available moisture forming the clear, viscous, colorless matrix you now know as ground substance.
4.4 Muscle Tissue and Motion
Learning Objectives
By the end of this section, you will be able to:
- Identify the three types of muscle tissue
- Compare and contrast the functions of each muscle tissue type
- Explain how muscle tissue can enable motion
Muscle tissue is characterized by properties that allow movement. Muscle cells are excitable; they respond to a stimulus. They are contractile, meaning they can shorten and generate a pulling force. When attached between two movable objects, in other words, bones, contractions of the muscles cause the bones to move. Some muscle movement is voluntary, which means it is under conscious control. For example, a person decides to open a book and read a chapter on anatomy. Other movements are involuntary, meaning they are not under conscious control, such as the contraction of your pupil in bright light. Muscle tissue is classified into three types according to structure and function: skeletal, cardiac, and smooth (Table 4.2).
Table 4.2 Comparison of Structure and Properties of Muscle Tissue Types
|
Tissue |
Histology |
Function |
Location |
|
Skeletal |
Long cylindrical fiber, striated, many peripherally located nuclei |
Voluntary movement, produces heat, protects organs |
Attached to bones and around entrance points to body (e.g., mouth, anus) |
|
Cardiac |
Short, branched, striated, single central nucleus |
Contracts to pump blood |
Heart |
|
Smooth |
Short, spindle-shaped, no evident striation, single nucleus in each fiber |
Involuntary movement, moves food, involuntary control of respiration, moves secretions, regulates flow of blood in arteries by contraction |
Walls of major organs and passageways |
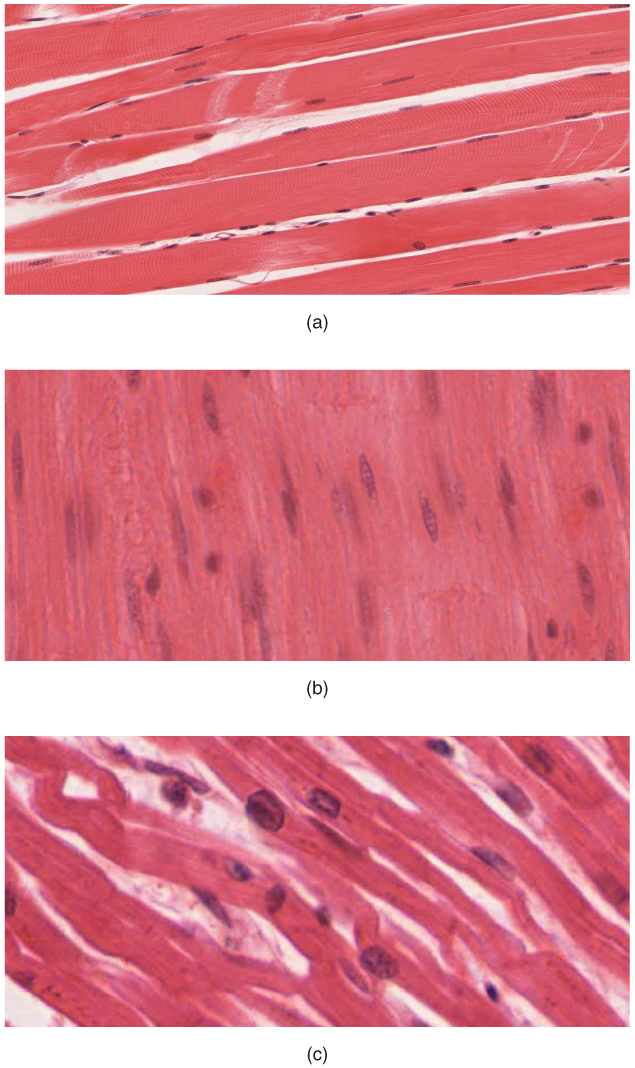
Skeletal muscle is attached to bones and its contraction makes possible locomotion, facial expressions, posture, and other voluntary movements of the body. Forty percent of your body mass is made up of skeletal muscle. Skeletal muscles generate heat as a byproduct of their contraction and thus participate in thermal homeostasis. Shivering is an involuntary contraction of skeletal muscles in response to perceived lower than normal body temperature. The muscle cell, or myocyte, develops from myoblasts derived from the mesoderm. Myocytes and their numbers remain relatively constant throughout life. Skeletal muscle tissue is arranged in bundles surrounded by connective tissue. Under the light microscope, muscle cells appear striated with many nuclei squeezed along the membranes. The striation is due to the regular alternation of the contractile proteins actin and myosin, along with the structural proteins that couple the contractile proteins to connective tissues. The cells are multinucleated as a result of the fusion of the many myoblasts that fuse to form each long muscle fiber.
Cardiac muscle forms the contractile walls of the heart. The cells of cardiac muscle, known as cardiomyocytes, also appear striated under the microscope. Unlike skeletal muscle fibers, cardiomyocytes are single cells typically with a single centrally located nucleus. A principal characteristic of cardiomyocytes is that they contract on their own intrinsic rhythms without any external stimulation. Cardiomyocyte attach to one another with specialized cell junctions called intercalated discs. Intercalated discs have both anchoring junctions and gap junctions. Attached cells form long, branching cardiac muscle fibers that are, essentially, a mechanical and electrochemical syncytium allowing the cells to synchronize their actions. The cardiac muscle pumps blood through the body and is under involuntary control. The attachment junctions hold adjacent cells together across the dynamic pressures changes of the cardiac cycle.
Smooth muscle tissue contraction is responsible for involuntary movements in the internal organs. It forms the contractile component of the digestive, urinary, and reproductive systems as well as the airways and arteries. Each cell is spindle shaped with a single nucleus and no visible striations (Figure 4.18).
Figure 4.18 Muscle Tissue (a) Skeletal muscle cells have prominent striation and nuclei on their periphery. (b) Smooth muscle cells have a single nucleus and no visible striations. (c) Cardiac muscle cells appear striated and have a single nucleus. (Micrographs provided by the Regents of University of Michigan Medical School © 2012)
Interactive Link
Watch this video to learn more about muscle tissue. In looking through a microscope how could you distinguish skeletal muscle tissue from smooth muscle?
4.5 Nervous Tissue Mediates Perception and Response
Learning Objectives
By the end of this section, you will be able to:
- Identify the classes of cells that make up nervous tissue
- Discuss how nervous tissue mediates perception and response
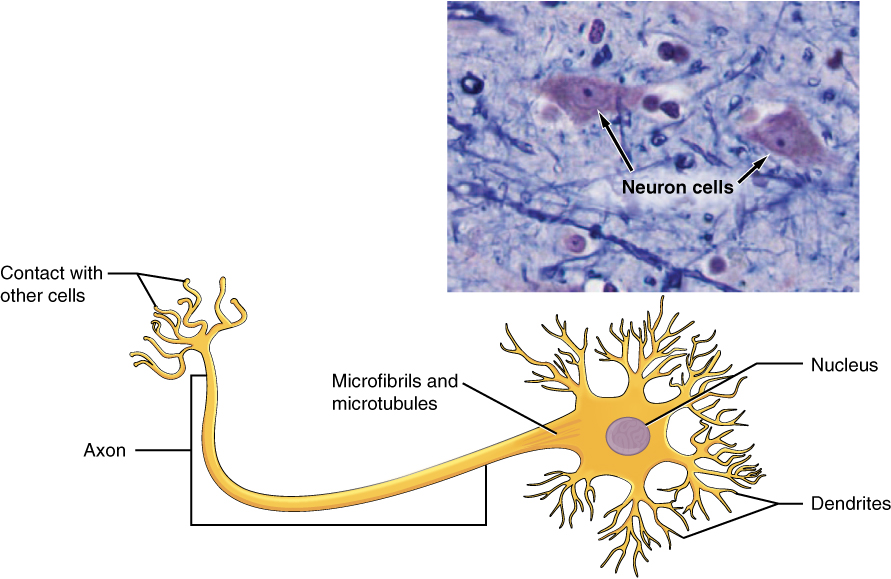
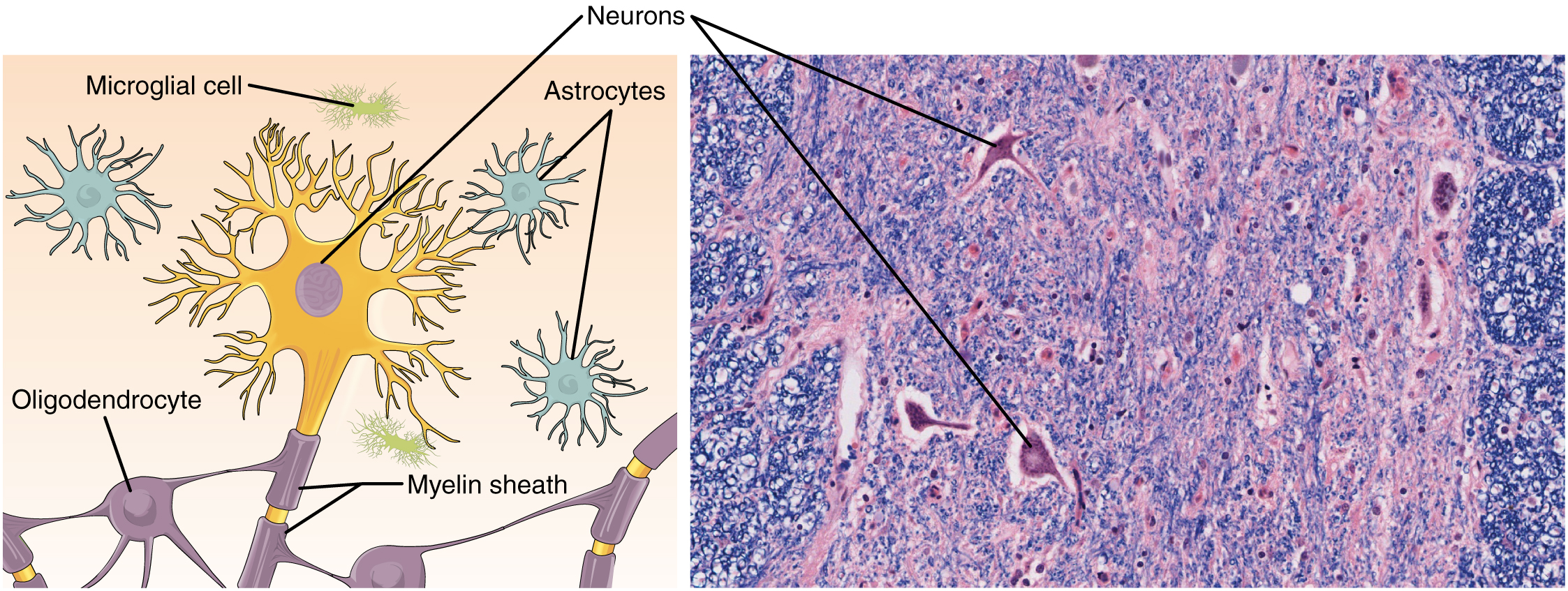
Nervous tissue is characterized as being excitable and capable of sending and receiving electrochemical signals that provide the body with information. Two main classes of cells make up nervous tissue: the neuron and neuroglia (Figure 4.19). Neurons propagate information via electrochemical impulses, called action potentials, which are biochemically linked to the release of chemical signals. Neuroglia play an essential role in supporting neurons and modulating their information propagation.
Figure 4.19 The Neuron The cell body of a neuron, also called the soma, contains the nucleus and mitochondria. The dendrites transfer the nerve impulse to the soma. The axon carries the action potential away to another excitable cell. LM × 1600. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Interactive Link
Follow this link to learn more about nervous tissue. What are the main parts of a nerve cell?
Neurons display distinctive morphology, well suited to their role as conducting cells, with three main parts. The cell body includes most of the cytoplasm, the organelles, and the nucleus. Dendrites branch off the cell body and appear as thin extensions. A long “tail,” the axon, extends from the neuron body and can be wrapped in an insulating layer known as myelin, which is formed by accessory cells. The synapse is the gap between nerve cells, or between a nerve cell and its target, for example, a muscle or a gland, across which the impulse is transmitted by chemical compounds known as neurotransmitters. When a neuron is sufficiently stimulated, it generates an action potential that propagates down the axon towards the synapse. If enough neurotransmitters are released at the synapse to stimulate the next neuron or target, a response is generated.
The second class of neural cells comprises the neuroglia or glial cells, which have been characterized as having a simple support role. The word “glia” comes from the Greek word for glue. Recent research is shedding light on the more complex role of neuroglia in the function of the brain and nervous system. Astrocyte cells, named for their distinctive star shape, are abundant in the central nervous system. The astrocytes have many functions, including regulation of ion concentration in the intercellular space, uptake and/or breakdown of some neurotransmitters, and formation of the blood-brain barrier, the membrane that separates the circulatory system from the brain. Microglia protect the nervous system against infection but are not nervous tissue because they are related to macrophages. Oligodendrocyte cells produce myelin in the central nervous system (brain and spinal cord) while the Schwann cell produces myelin in the peripheral nervous system (Figure 4.20).
Figure 4.20 Nervous Tissue Nervous tissue is made up of neurons and neuroglia. The cells of nervous tissue are specialized to transmit and receive impulses. LM × 872. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
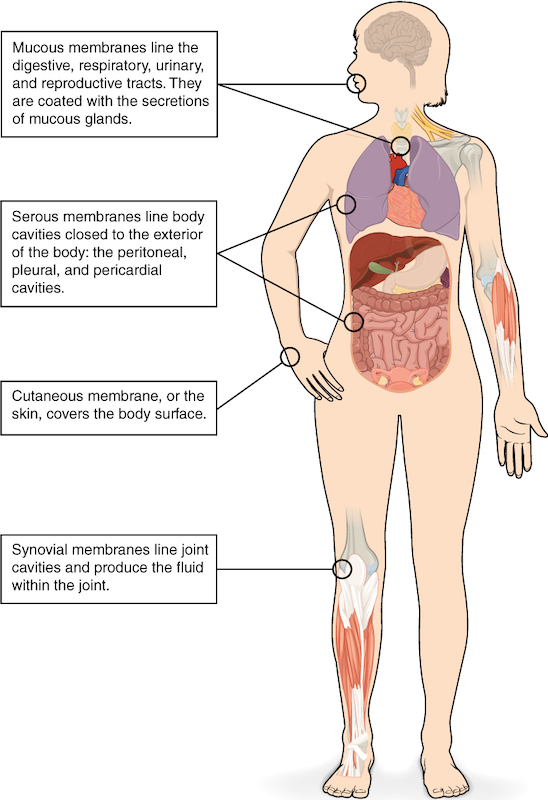
Body Membranes
A tissue membrane is a thin layer or sheet of cells that covers the outside of the body (for example, skin), the organs (for example, pericardium), internal passageways that lead to the exterior of the body (for example, mucosa of stomach), and the lining of the moveable joint cavities. There are two basic types of tissue membranes: connective tissue membranes and epithelial membranes (Figure 4.4).
Figure 4.4 Tissue Membranes The two broad categories of tissue membranes in the body are (1) connective tissue membranes, which include synovial membranes, and (2) epithelial membranes, which include mucous membranes, serous membranes, and the cutaneous membrane, in other words, the skin.
Connective Tissue Membranes
The connective tissue membrane is formed solely from connective tissue. These membranes encapsulate organs, such as the kidneys, and line our movable joints. A synovial membrane is a type of connective tissue membrane that lines the cavity of a freely movable joint. For example, synovial membranes surround the joints of the shoulder, elbow, and knee. Fibroblasts in the inner layer of the synovial membrane release hyaluronan into the joint cavity. The hyaluronan effectively traps available water to form the synovial fluid, a natural lubricant that enables the bones of a joint to move freely against one another without much friction. This synovial fluid readily exchanges water and nutrients with blood, as do all body fluids.
Epithelial Membranes
The epithelial membrane is composed of epithelium attached to a layer of connective tissue, for example, your skin. The skin is an epithelial membrane also called the cutaneous membrane. It is a stratified squamous epithelial membrane resting on top of connective tissue. The apical surface of this membrane is exposed to the external environment and is covered with dead, keratinized cells that help protect the body from desiccation and pathogens.
The mucous membrane is also a composite of connective and epithelial tissues. Sometimes called mucosae, these epithelial membranes line the body cavities and hollow passageways that open to the external environment, and include the digestive, respiratory, excretory, and reproductive tracts. Mucus, produced by the epithelial exocrine glands, covers the epithelial layer. The underlying connective tissue, called the lamina propria (literally “own layer”), help support the fragile epithelial layer.Serous Membranes
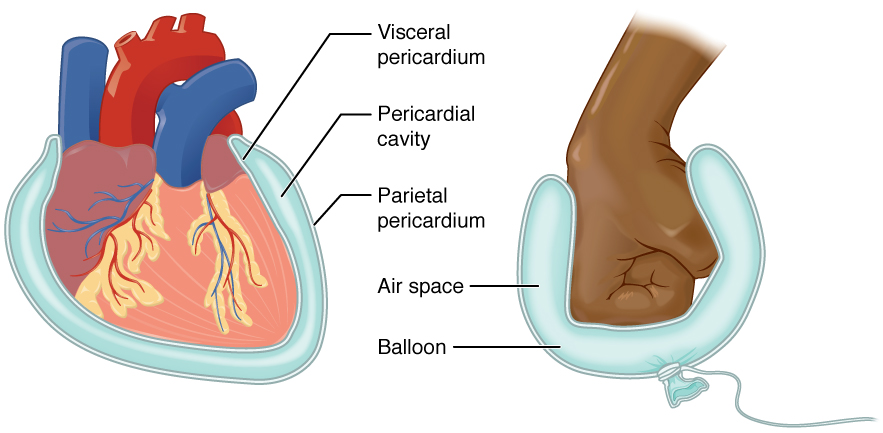
A serous membrane (also referred to a serosa) is one of the thin membranes that cover the walls and organs in the thoracic and abdominopelvic cavities. The parietal layers of the membranes line the walls of the body cavity (pariet- refers to a cavity wall). The visceral layer of the membrane covers the organs (the viscera). Between the parietal and visceral layers is a very thin, fluid-filled serous space, or cavity (Figure 1.17).
Figure 1.17 Serous Membrane Serous membrane lines the pericardial cavity and reflects back to cover the heart—much the same way that an underinflated balloon would form two layers surrounding a fist.
There are three serous cavities and their associated membranes. The pleura is the serous membrane that encloses the pleural cavity; the pleural cavity surrounds the lungs. The pericardium is the serous membrane that encloses the pericardial cavity; the pericardial cavity surrounds the heart. The peritoneum is the serous membrane that encloses the peritoneal cavity; the peritoneal cavity surrounds several organs in the abdominopelvic cavity. The serous membranes form fluid-filled sacs, or cavities, that are meant to cushion and reduce friction on internal organs when they move, such as when the lungs inflate or the heart beats. Both the parietal and visceral serosa secrete the thin, slippery serous fluid located within the serous cavities. The pleural cavity reduces friction between the lungs and the body wall. Likewise, the pericardial cavity reduces friction between the heart and the wall of the pericardium. The peritoneal cavity reduces friction between the abdominal and pelvic organs and the body wall. Therefore, serous membranes provide additional protection to the viscera they enclose by reducing friction that could lead to inflammation of the organs.
Tissue and Aging
According to poet Ralph Waldo Emerson, “The surest poison is time.” In fact, biology confirms that many functions of the body decline with age. All the cells, tissues, and organs are affected by senescence, with noticeable variability between individuals owing to different genetic makeup and lifestyles. The outward signs of aging are easily recognizable. The skin and other tissues become thinner and drier, reducing their elasticity, contributing to wrinkles and high blood pressure. Hair turns gray because follicles produce less melanin, the brown pigment of hair and the iris of the eye. The face looks flabby because elastic and collagen fibers decrease in connective tissue and muscle tone is lost. Glasses and hearing aids may become parts of life as the senses slowly deteriorate, all due to reduced elasticity. Overall height decreases as the bones lose calcium and other minerals. With age, fluid decreases in the fibrous cartilage disks intercalated between the vertebrae in the spine. Joints lose cartilage and stiffen. Many tissues, including those in muscles, lose mass through a process called atrophy. Lumps and rigidity become more widespread. As a consequence, the passageways, blood vessels, and airways become more rigid. The brain and spinal cord lose mass. Nerves do not transmit impulses with the same speed and frequency as in the past. Some loss of thought clarity and memory can accompany aging. More severe problems are not necessarily associated with the aging process and may be symptoms of underlying illness.
As exterior signs of aging increase, so do the interior signs, which are not as noticeable. The incidence of heart diseases, respiratory syndromes, and type 2 diabetes increases with age, though these are not necessarily age-dependent effects. Wound healing is slower in the elderly, accompanied by a higher frequency of infection as the capacity of the immune system to fend off pathogen declines.
Aging is also apparent at the cellular level because all cells experience changes with aging. Telomeres, regions of the chromosomes necessary for cell division, shorten each time cells divide. As they do, cells are less able to divide and regenerate. Because of alterations in cell membranes, transport of oxygen and nutrients into the cell and removal of carbon dioxide and waste products from the cell are not as efficient in the elderly. Cells may begin to function abnormally, which may lead to diseases associated with aging, including arthritis, memory issues, and some cancers.
The progressive impact of aging on the body varies considerably among individuals, but Studies indicate, however, that exercise and healthy lifestyle choices can slow down the deterioration of the body that comes with old age.
Homeostatic Imbalances: Tissues and Cancer
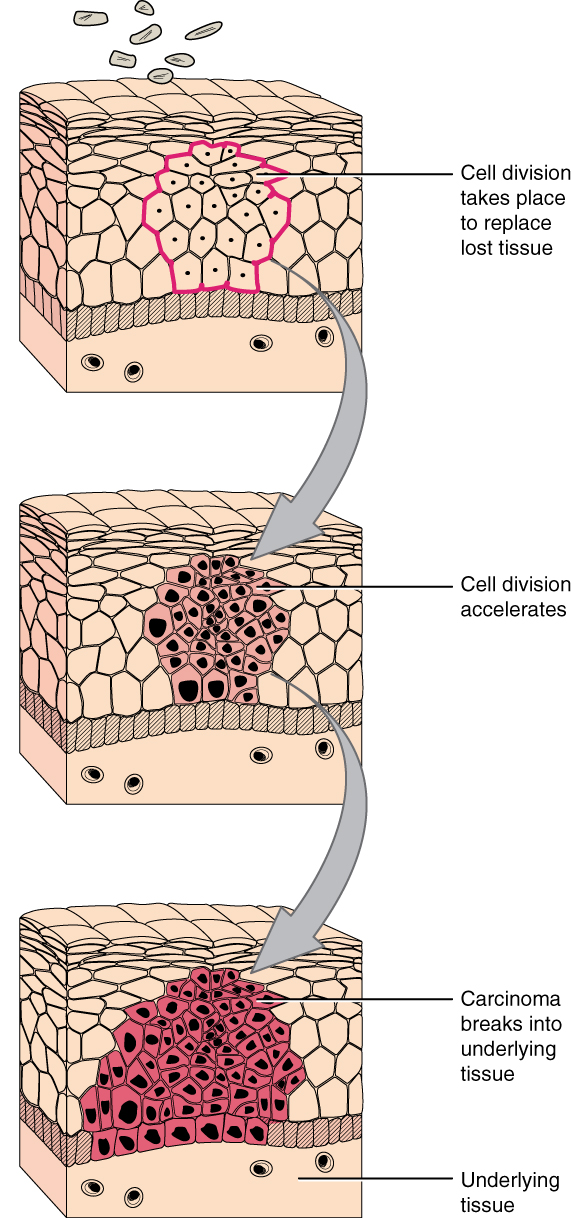
Cancer is a generic term for many diseases in which cells escape regulatory signals. Uncontrolled growth, invasion into adjacent tissues, and colonization of other organs, if not treated early enough, are its hallmarks. Health suffers when tumors “rob” blood supply from the “normal” organs.
A mutation is defined as a permanent change in the DNA of a cell. Epigenetic modifications, changes that do not affect the code of the DNA but alter how the DNA is decoded, are also known to generate abnormal cells. Alterations in the genetic material may be caused by environmental agents, infectious agents, or errors in the replication of DNA that accumulate with age. Many mutations do not cause any noticeable change in the functions of a cell. However, if the modification affects key proteins that have an impact on the cell’s ability to proliferate in an orderly fashion, the cell starts to divide abnormally. As changes in cells accumulate, they lose their ability to form regular tissues. A tumor, a mass of cells displaying abnormal architecture, forms in the tissue. Many tumors are benign, meaning they do not metastasize nor cause disease. A tumor becomes malignant, or cancerous, when it breaches the confines of its tissue, promotes angiogenesis, attracts the growth of capillaries, and metastasizes to other organs (Figure 4.22). The specific names of cancers reflect the tissue of origin. Cancers derived from epithelial cells are referred to as carcinomas. Cancer in myeloid tissue or blood cells form myelomas. Leukemias are cancers of white blood cells, whereas sarcomas derive from connective tissue. Cells in tumors differ both in structure and function. Some cells, called cancer stem cells, appear to be a subtype of cell responsible for uncontrolled growth. Recent research shows that contrary to what was previously assumed, tumors are not disorganized masses of cells, but have their own structures.
Figure 4.22 Development of Cancer Note the change in cell size, nucleus size, and organization in the tissue.
Interactive Link
Watch this video to learn more about tumors. What is a tumor?
Cancer treatments vary depending on the disease’s type and stage. Traditional approaches, including surgery, radiation, chemotherapy, and hormonal therapy, aim to remove or kill rapidly dividing cancer cells, but these strategies have their limitations. Depending on a tumor’s location, for example, cancer surgeons may be unable to remove it. Radiation and chemotherapy are difficult, and it is often impossible to target only the cancer cells. The treatments inevitably destroy healthy tissue as well. To address this, researchers are working on pharmaceuticals that can target specific proteins implicated in cancer-associated molecular pathways.
Chapter Review
4.1 Types of Tissues
The human body contains more than 200 types of cells that can all be classified into four types of tissues: epithelial, connective, muscle, and nervous. Epithelial tissues act as coverings controlling the movement of materials across the surface. Connective tissue integrates the various parts of the body and provides support and protection to organs. Muscle tissue allows the body to move. Nervous tissues propagate information.
The study of the shape and arrangement of cells in tissue is called histology.
Different types of tissues form membranes that enclose organs, provide a friction-free interaction between organs, and keep organs together. Synovial membranes are connective tissue membranes that protect and line the joints. Epithelial membranes are formed from epithelial tissue attached to a layer of connective tissue. There are three types of epithelial membranes: mucous, which contain glands; serous, which secrete fluid; and cutaneous which makes up the skin.
4.2 Epithelial Tissue
In epithelial tissue, cells are closely packed with little or no extracellular matrix except for the basal lamina that separates the epithelium from underlying tissue. The main functions of epithelia are protection from the environment, coverage, secretion and excretion, absorption, and filtration. Cells are bound together by tight junctions that form an impermeable barrier. They can also be connected by gap junctions, which allow free exchange of soluble molecules between cells, and anchoring junctions, which attach cell to cell or cell to matrix. The different types of epithelial tissues are characterized by their cellular shapes and arrangements: squamous, cuboidal, or columnar epithelia. Single cell layers form simple epithelia, whereas stacked cells form stratified epithelia. Very few capillaries penetrate these tissues.
Glands are secretory tissues and organs that are derived from epithelial tissues. Exocrine glands release their products through ducts. Endocrine glands secrete hormones directly into the interstitial fluid and blood stream. Glands are classified both according to the type of secretion and by their structure.
4.3 Connective Tissue Supports and Protects
Connective tissue is a heterogeneous tissue with many cell shapes and tissue architecture. Structurally, all connective tissues contain cells that are embedded in an extracellular matrix stabilized by proteins. The chemical nature and physical layout of the extracellular matrix and proteins vary enormously among tissues, reflecting the variety of functions that connective tissue fulfills in the body. Connective tissues separate and cushion organs, protecting them from shifting or traumatic injury. Connect tissues provide support and assist movement, store and transport energy molecules, protect against infections, and contribute to temperature homeostasis.
Many different cells contribute to the formation of connective tissues. Fibroblasts are the most abundant and secrete many protein fibers, adipocytes specialize in fat storage, hematopoietic cells from the bone marrow give rise to all the blood cells, chondrocytes form cartilage, and osteocytes form bone. The extracellular matrix contains fluid, proteins, polysaccharide derivatives, and, in the case of bone, mineral crystals. Protein fibers fall into three major groups: collagen fibers that are thick, strong, flexible, and resist stretch; reticular fibers that are thin and form a supportive mesh; and elastin fibers that are thin and elastic.
The major types of connective tissue are connective tissue proper, supportive tissue, and fluid tissue. Loose connective tissue proper includes adipose tissue, areolar tissue, and reticular tissue. These serve to hold organs and other tissues in place and, in the case of adipose tissue, isolate and store energy reserves. The matrix is the most abundant feature for loose tissue although adipose tissue does not have much extracellular matrix. Dense connective tissue proper is richer in fibers and may be regular, with fibers oriented in parallel as in ligaments and tendons, or irregular, with fibers oriented in several directions. Organ capsules (collagenous type) and walls of arteries (elastic type) contain dense irregular connective tissue. Cartilage and bone are supportive tissue. Cartilage contains chondrocytes and is somewhat flexible. Hyaline cartilage is smooth and clear, covers joints, and is found in the growing portion of bones. Fibrocartilage is tough because of extra collagen fibers and forms, among other things, the intervertebral discs. Elastic cartilage can stretch and recoil to its original shape because of its high content of elastic fibers. The matrix contains very few blood vessels. Bones are made of a rigid, mineralized matrix containing calcium salts, crystals, and osteocytes lodged in lacunae. Bone tissue is highly vascularized. Cancellous bone is spongy and less solid than compact bone. Fluid tissue, for example blood and lymph, is characterized by a liquid matrix and no supporting fibers.
4.4 Muscle Tissue and Motion
The three types of muscle cells are skeletal, cardiac, and smooth. Their morphologies match their specific functions in the body. Skeletal muscle is voluntary and responds to conscious stimuli. The cells are striated and multinucleated appearing as long, unbranched cylinders. Cardiac muscle is involuntary and found only in the heart. Each cell is striated with a single nucleus and they attach to one another to form long fibers. Cells are attached to one another at intercalated disks. The cells are interconnected physically and electrochemically to act as a syncytium. Cardiac muscle cells contract autonomously and involuntarily. Smooth muscle is involuntary. Each cell is a spindle-shaped fiber and contains a single nucleus. No striations are evident because the actin and myosin filaments do not align in the cytoplasm.
4.5 Nervous Tissue Mediates Perception and Response
The most prominent cell of the nervous tissue, the neuron, is characterized mainly by its ability to receive stimuli and respond by generating an electrical signal, known as an action potential, which can travel rapidly over great distances in the body. A typical neuron displays a distinctive morphology: a large cell body branches out into short extensions called dendrites, which receive chemical signals from other neurons, and a long tail called an axon, which relays signals away from the cell to other neurons, muscles, or glands. Many axons are wrapped by a myelin sheath, a lipid derivative that acts as an insulator and speeds up the transmission of the action potential. Other cells in the nervous tissue, the neuroglia, include the astrocytes, microglia, oligodendrocytes, and Schwann cells.
4.6 Tissue Aging
Age affects all the tissues and organs of the body. Damaged cells do not regenerate as rapidly as in younger people. Perception of sensation and effectiveness of response are lost in the nervous system. Muscles atrophy, and bones lose mass and become brittle. Collagen decreases in some connective tissue, and joints stiffen.
Key Terms
adipocytes: lipid storage cells
adipose tissue: specialized areolar tissue rich in stored fat
Desmosome/anchoring junction : mechanically attaches adjacent cells to each other or to the basement membrane
apical: that part of a cell or tissue which, in general, faces an open space
areolar tissue: (also, loose connective tissue) a type of connective tissue proper that shows little specialization with cells dispersed in the matrix
astrocyte: star-shaped cell in the central nervous system that regulates ions and uptake and/or breakdown of some neurotransmitters and contributes to the formation of the blood-brain barrier
atrophy: loss of mass and function
basement membrane: in epithelial tissue, a thin layer of fibrous material that anchors the epithelial tissue to the underlying connective tissue; made up of the basal lamina and reticular lamina
cardiac muscle: heart muscle, under involuntary control, composed of striated cells that attach to form fibers, each cell contains a single nucleus, contracts autonomously
cell junction: point of cell-to-cell contact that connects one cell to another in a tissue
chondrocytes: cells of the cartilage
collagen fiber: flexible fibrous proteins that give connective tissue tensile strength
connective tissue: type of tissue that serves to hold in place, connect, and integrate the body’s organs and systems
connective tissue membrane: connective tissue that encapsulates organs and lines movable joints
connective tissue proper: connective tissue containing a viscous matrix, fibers, and cells.
cutaneous membrane: skin; epithelial tissue made up of a stratified squamous epithelial cells that cover the outside of the body
dense connective tissue: connective tissue proper that contains many fibers that provide both elasticity and protection
elastic cartilage: type of cartilage, with elastin as the major protein, characterized by rigid support as well as elasticity
elastic fiber: fibrous protein within connective tissue that contains a high percentage of the protein elastin that allows the fibers to stretch and return to original size
endocrine gland: groups of cells that release chemical signals into the intercellular fluid to be picked up and transported to their target organs by blood
endothelium: tissue that lines vessels of the lymphatic and cardiovascular system, made up of a simple squamous epithelium
epithelial membrane: epithelium attached to a layer of connective tissue
epithelial tissue: type of tissue that serves primarily as a covering or lining of body parts, protecting the body; it also functions in absorption, transport, and secretion
exocrine gland: group of epithelial cells that secrete substances through ducts that open to the skin or to internal body surfaces that lead to the exterior of the body
fibroblast: most abundant cell type in connective tissue, secretes protein fibers and matrix into the extracellular space
fibrocartilage: tough form of cartilage, made of thick bundles of collagen fibers embedded in chondroitin sulfate ground substance
fibrocyte: less active form of fibroblast
fluid connective tissue: specialized cells that circulate in a watery fluid containing salts, nutrients, and dissolved proteins
gap junction: allows cytoplasmic communications to occur between cells
goblet cell: unicellular gland found in columnar epithelium that secretes mucous
ground substance: fluid or semi-fluid portion of the matrix
histamine: chemical compound released by mast cells in response to injury that causes vasodilation and endothelium permeability
histology: microscopic study of tissue architecture, organization, and function
hyaline cartilage: most common type of cartilage, smooth and made of short collagen fibers embedded in a chondroitin sulfate ground substance
inflammation: response of tissue to injury
lacunae: (singular = lacuna) small spaces in bone or cartilage tissue that cells occupy
loose connective tissue: (also, areolar tissue) type of connective tissue proper that shows little specialization with cells dispersed in the matrix
matrix: extracellular material which is produced by the cells embedded in it, containing ground substance and fibers
mucous gland: group of cells that secrete mucous, a thick, slippery substance that keeps tissues moist and acts as a lubricant
mucous membrane: tissue membrane that is covered by protective mucous and lines tissue exposed to the outside environment
muscle tissue: type of tissue that is capable of contracting and generating tension in response to stimulation; produces movement.
myelin: layer of lipid inside some neuroglial cells that wraps around the axons of some neurons
myocyte: muscle cells
necrosis: accidental death of cells and tissues
nervous tissue: type of tissue that is capable of sending and receiving impulses through electrochemical signals.
neuroglia: supportive neural cells
neuron: excitable neural cell that transfer nerve impulses
oligodendrocyte: neuroglial cell that produces myelin in the brain
pseudostratified columnar epithelium: tissue that consists of a single layer of irregularly shaped and sized cells that give the appearance of multiple layers; found in ducts of certain glands and the upper respiratory tract
reticular fiber: fine fibrous protein, made of collagen subunits, which cross-link to form supporting “nets” within connective tissue
reticular lamina: matrix containing collagen and elastin secreted by connective tissue; a component of the basement membrane
reticular tissue: type of loose connective tissue that provides a supportive framework to soft organs, such as lymphatic tissue, spleen, and the liver
Schwann cell: neuroglial cell that produces myelin in the peripheral nervous system
serous gland: group of cells within the serous membrane that secrete a lubricating substance onto the surface
serous membrane: type of tissue membrane that lines body cavities and lubricates them with serous fluid
simple columnar epithelium: tissue that consists of a single layer of column-like cells; promotes secretion and absorption in tissues and organs
simple cuboidal epithelium: tissue that consists of a single layer of cube-shaped cells; promotes secretion and absorption in ducts and tubules
simple squamous epithelium: tissue that consists of a single layer of flat scale-like cells; promotes diffusion and filtration across surface
skeletal muscle: usually attached to bone, under voluntary control, each cell is a fiber that is multinucleated and striated
smooth muscle: under involuntary control, moves internal organs, cells contain a single nucleus, are spindle-shaped, and do not appear striated; each cell is a fiber
stratified columnar epithelium: tissue that consists of two or more layers of column-like cells, contains glands and is found in some ducts
stratified cuboidal epithelium: tissue that consists of two or more layers of cube-shaped cells, found in some ducts
stratified squamous epithelium: tissue that consists of multiple layers of cells with the most apical being flat scale-like cells; protects surfaces from abrasion
striation: alignment of parallel actin and myosin filaments which form a banded pattern
supportive connective tissue: type of connective tissue that provides strength to the body and protects soft tissue
synovial membrane: connective tissue membrane that lines the cavities of freely movable joints, producing synovial fluid for lubrication
tight junction: forms an impermeable barrier between cells
tissue: group of cells that are similar in form and perform related functions
tissue membrane: thin layer or sheet of cells that covers the outside of the body, organs, and internal cavities
transitional epithelium: form of stratified epithelium found in the urinary tract, characterized by an apical layer of cells that change shape in response to the presence of urine
Critical Thinking Questions
31. Identify the four types of tissue in the body, and describe the major functions of each tissue.
33. What is the function of synovial membranes?
34. The structure of a tissue usually is optimized for its function. Describe how the structure of the mucosa and its cells match its function of nutrient absorption.
35. One of the main functions of connective tissue is to integrate organs and organ systems in the body. Discuss how blood fulfills this role.
36. Why does an injury to cartilage, especially hyaline cartilage, heal much more slowly than a bone fracture?
38. Why does skeletal muscle look striated?
39. Which morphological adaptations of neurons make them suitable for the transmission of nerve impulse?
40. What are the functions of astrocytes?
43. As an individual ages, a constellation of symptoms begins the decline to the point where an individual’s functioning is compromised. Identify and discuss two factors that have a role in factors leading to the compromised situation.
44. Discuss changes that occur in cells as a person ages.